Introduction With health and social care services striving to address the challenge of demographic change and rising demands on public services, falls among older people are a major and growing concern. A recently published economic evaluation provided an estimate of the cost to health and social care services in Scotland of managing the consequences of falls: in excess of £470 million and set to rise over the next decade as our population ages and the proportion with multimorbidity and polypharmacy grows. Less easy to quantify is the impact of falls on an older person's independence and quality of life, and the repercussions for family and friends.However, falls are not an inevitable consequence of old age. Well-organised services, delivering recommended and evidence based practices can prevent many falls and fractures in older people in the community setting.Background Since 2010 the National Falls Programme has aimed to support health and social care partnership areas to implement local integrated pathways which enable a systematic and evidence based approach to falls prevention and management. The model pathway is outlined in the Healthcare Improvement Scotland resource, Up and About.The 2012 report, Up and About or Falling Short, presented the findings of a mapping exercise in Scotland which aimed to identify the extent to which recommended practices were embedded in systems of care for older people. The report suggested that although in recent years there has been progress in the implementation of local care pathways for older people who have fallen, there remains variation in service provision and quality in Scotland. An older person's likelihood of being offered evidence based care depends on where and to whom he or she presents following a fall or with a fall-related injury. Opportunities for prevention of falls and fractures are being missed.The Framework for Action The Framework for Action builds on the model presented in the Up and About resource, and focuses on falls prevention and management and fracture prevention for older people living in the community. The Framework is underpinned by evidence from research and draws on knowledge and experience gained by the falls prevention community in Scotland over the last four years. It identifies and describes key actions for health and social care services at each of the four stages of the pathway. These actions represent the minimum standard of care an older person should expect to receive, regardless of where and when they present to services. The Framework provides a road map for developing or enhancing a falls pathway.Scotland is a rich source of examples of successful implementation of the majority of these actions. A number of these examples will be available on the Falls and Bone Health Community pages on the Knowledge Network (http://www.knowledge.scot.nhs.uk/fallsandbonehealth.aspx currently under further development).Development of the Framework for Action The Framework for Action was developed as part of the National Falls Programme by the National Programme Manager in partnership with CH©P Falls Leads representing all partnership areas in Scotland and other key stakeholders. It is informed by recommendations and evidence from current published guidance and research and the tacit knowledge of health and social care professionals with subject matter knowledge and experience.Assessing where you are A self assessment tool will be available to enable partnerships to identify the extent to which recommended practices to prevent and manage falls and prevent fragility fractures are embedded in their systems of care for older people. This information can be used to identify progress and potential areas for further improvement.
Royal College of Physicians of Edinburgh
Response to the Scottish government on the Prevention and Management of Falls in the Community: a Framework for Action for Scotland 2014/2015
The Royal College of Physicians of Edinburgh (the College) is pleased to respond to the call for views on the Scottish Government’s Prevention and Management of Falls in the Community: a Framework for Action for Scotland 2014/2015.
General Comments:
The aims of the framework are to create a minimum standard of care for community dwelling older people who sustain a fall or are at risk of falling. It draws from evidence on falls prevention from meta-analysis, systematic reviews and relevant falls prevention service initiatives that have been established in Scotland and elsewhere. There is a focus on triage of older people who have fallen to a stepped level of assessment. This strategy should provide all older people who fall with access to a minimum assessment. However, the success of implementation relies on a wide range of people in both health and social care settings having training in identifying those who have fallen or proactively enquiring about fall risk factors.
The document currently concentrates on identification and screening of individuals who fall. There is proportionally less documentation on evidence based interventions following the screening process. Acknowledgement of the resources required to implement intervention is important as many falls prevention interventions include a prolonged exercise component (minimum of 50 hours). To achieve this will require explicit resource allocation.
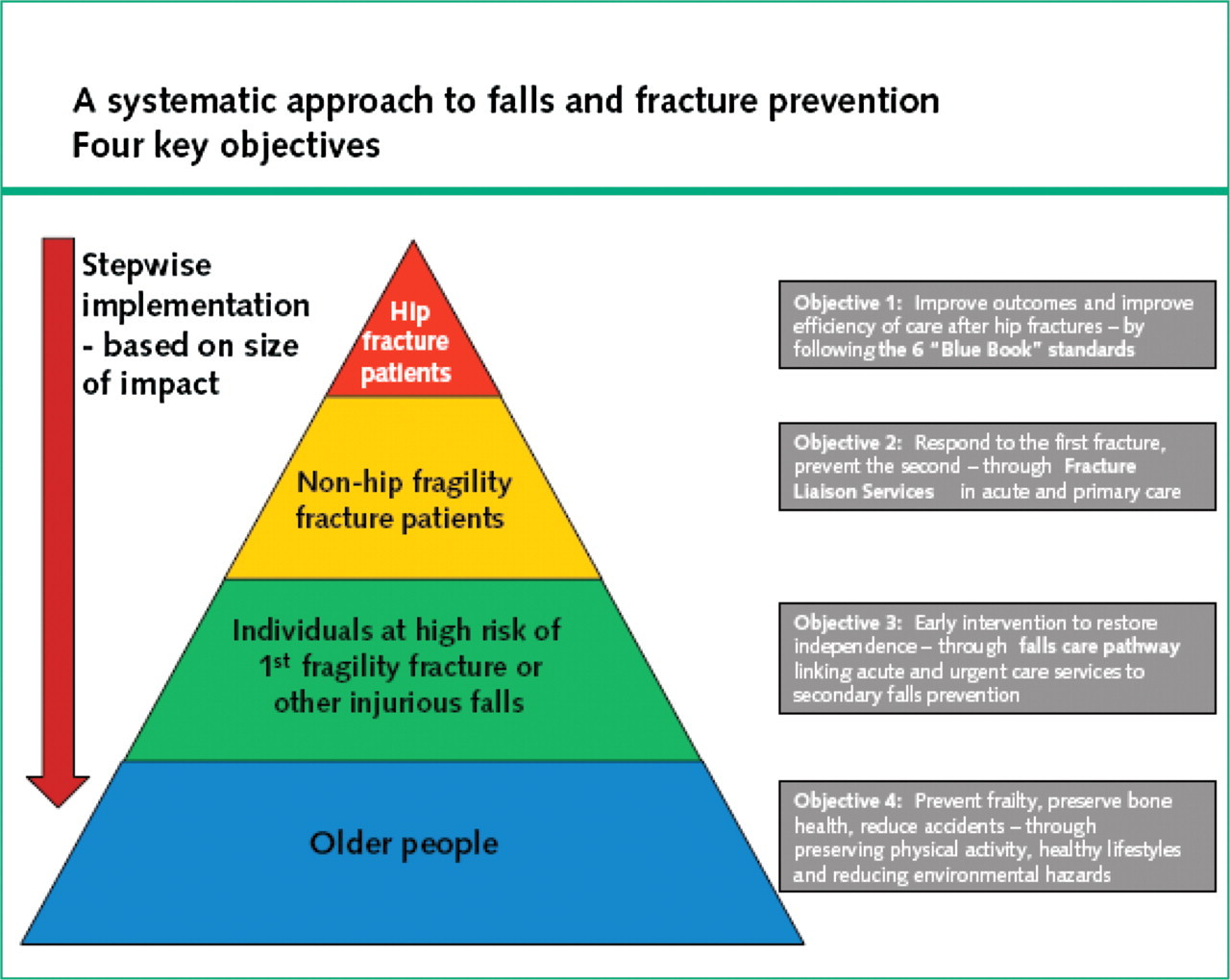
College Fellows have suggested that more emphasis should be placed on the pyramid approach (illustrated below) to dealing with falls and fracture prevention ie start with those who have already had a fall-related fracture for whom the benefits will be greatest, and work down. The pyramid system has been adopted by services in England and other countries and ensures that resources are targeted at those at high risk and those most likely to benefit. In times when resources are tightly constrained and efficient and effective models are sought, the College suggests further consideration is given to this approach.
Martin F. Next steps for fall and fracture prevention. Age Ageing 2009;38:640-643.
Comments on specific points in the draft framework:
Stage 1: Supporting health improvement and self-management to reduce the risk of falls and fragility fractures
Action 1.1
Up to date information on the prevention of falls and the prevention of harm from falls is made available to older people health and social care services.
Comment:
Generally agree with this point; however greater clarity is required about how this information is to be produced, standardised and distributed. Is it proposed to replace existing documents with a single standardised falls information document? How will this be maintained, updated, resourced and distributed?
Stage 2: Identifying individuals at high risk of falls and/or fragility fractures
Action 2.1
Level 1 assessment is offered to older people who report a fall or an injury or functional decline caused by a fall.
Comment:
Level 1 assessment is different from NICE clinical guidance (CG161) which recommends that older people who present for medical attention due to a fall or fall related injury should be offered a multifactorial falls risk assessment. NICE recommends that this is performed by a healthcare professional with appropriate skills or experience. The model proposed relies on a range of individuals within health and social care services who may not have experience of managing older people with falls. Those responsible for administering level 1 assessment will require training to ensure at risk individuals are referred on for more detailed assessment.
Level 1 assessment questions (detailed in Appendix 1) will require greater specificity of actions to be undertaken, and the actions of the individual performing the screening should be directed more specifically eg anyone reporting a blackout should be referred for specialist assessment (Level 3).
Action 2.2
Everyone identified at high risk of further falls by Level 1 assessment is offered intervention to identify and address possible contributory factors – Level 2 assessment
Comment:
Agree that those at higher risk of falls should have a more detailed falls assessment. This should be evidence based.
Stage 3: Responding to an individual who has just fallen and requires immediate assistance
Action 3.1
Responding services have a standard operating procedure for responding to people who have fallen and have or have not sustained injuries.
Comment:
Agree with stated principles behind SOP. However, the specifics need defining.
Action 3.3
Responding services have a standard operating procedure for identifying and meeting the immediate needs of a person who has fallen.
Comment:
Agree with standardising procedure to address immediate needs. SOP should include ascertainment of any injury sustained, determining if loss of consciousness has occurred, exclude head injury and fracture. SOP should also have simple determinants of cognition, infection, concomitant medical condition such as acute coronary syndrome or stroke, which would require urgent medical assessment. If an injury has been sustained there should be a mechanism to ensure that the older person has access to a higher level assessment for the cause of the fall, even if not conveyed.
Action 3.4
Health and social care services working with older people in their own homes (including care homes) have a standard operating procedure to identify and meet the immediate need of an older person who falls in their presence or is found on the floor.
Comment:
Agree with recommendation that an SOP is in situ for these circumstances. As per 3.3. there is a need for this SOP to triage individuals into those who require immediate medical assessment for their injuries, and those who can wait for a later assessment of both their injury and any fall risk factors.
Action 3.5
Older people presenting to responding services following a fall and who are not conveyed to hospital, are offered Level 1 assessment.
Comment:
Agree that offering access to a falls assessment is important for this group. If the fall has been sufficient to warrant calling a responding services, this individual is likely to be at higher risk of future falls and Level 2 assessment would be more appropriate.
Action 3.6
Older people assisted by other health and social care services in the event of a fall, and who are not conveyed to hospital, are offered Level 1 assessment.
Comment:
The College recommends a higher level assessment is used in this situation, as per NICE CG 161, and that the assessment if performed by someone experienced in falls risk assessment with a full multifactorial assessment.
Stage 4: Co-ordinated management including specialist assessment
Action 4.1
Older people identified at high risk of further falls are offered a Level 2 assessment
Comment:
Agree that those at high risk of further falls should have assessment performed of greater detail. NICE CG161 indicates this should be offered by a specialist falls service.
Action 4.2
Health and social care services providing Level 2 assessment have a governance infrastructure to ensure suitable staff undertake Level 2 assessments.
Comment:
NICE CG161 recommends that a multifactorial assessment is performed for those at risk of future falls. This should be performed by a health professional with skills and experience in falls prevention. Multifactorial studies in falls prevention which have used a single individual to perform falls prevention assessment and intervention have not demonstrated significant reduction in future falls. By contrast, multifactorial assessment and intervention performed by a combination of physiotherapists, occupational therapists and physicians has proven to effectively reduce fall rates.
Action 4.3
Following Level 2 assessment, the person is provided with a personalised Falls and Fracture Prevention Action Plan.
Comment:
Agree with the objective to provide an individualised intervention plan following multifactorial falls risk assessment. However, there are outstanding questions:
- How will the action plan be implemented?
- Who is going to do so?
- What timescale is this to be in?
Action 4.4
Level 3 assessment and remedial interventions offered are in line with current and emerging evidence
Comment:
Specialised falls intervention is part of the recommendation for all individuals who sustain a fall and come to the attention of health professionals. How will the Level 3 intervention be defined?
Action 4.5
Following Level 2 assessment there are referral pathways into services that provide evidence based assessment (Level 3) and intervention.
Comment:
Agree that there should be access to services which provide evidence based assessment and intervention. However, all older people who fall should have access to services which provide evidence based assessment and intervention.
How will the exercise intervention be resourced? 50 hours has been determined to be the effective duration of exercise to lead to significant reduction in future falls. To achieve this universally will require directed resource.
Action 4.6
Services providing Level 2 assessment can refer directly into services that provide evidence base assessment (Level 3) and intervention.
Comment:
Agree that any triage system that is introduced should have clearly defined parameters linked to direct access to specialist falls prevention assessment and intervention that is evidence based. There should not be additional administrative or financial barriers to accessing services which have been shown to be clinically effective.
Action 4.7
There is a quality assurance process which monitors whether or not Falls and Fracture Prevention Action Plans are implemented.
Comment:
Agree that there should be facility to monitor whether Action Plans are being implemented. If such a monitoring process is being introduced, this would be an opportunity to determine relevant clinical outcomes ie are Action Plans leading to a reduction in future falls, fall injuries, fractures and primary and secondary care service use?
