Introduction
We address this topic from the perspective of a local public health team in Scotland’s largest health board. Did we make any decisions at local level or did we just struggle to implement decisions, policy and guidance decided at national or international level? We made decisions about individual outbreaks, isolation in individual cases, local standard operating procedures, but less so on guidance or policy. Our experience in this context was that local public health teams, via the Scottish directors of public health, the National Incident Management Team and other national groups, were able to influence decisions and policy in a way not previously seen in Scotland. There was a real willingness by civil servants, government medical officers and policymakers to seek our views and to enable us to influence policy and strategy. In the long term, this investment in these relationships will be good for Scottish public health and for the country because it will strengthen the voice of prevention and equity in policy decisions.
There was another side to this, some may say an inevitability in a time of crisis. There were many occasions when the first time we, in local public health teams, heard of a change in policy was from a press conference by our political leaders. There was then an expectation that this new policy be implemented within a few days. This was a major challenge for local teams, made more stressful by criticism in the media that we hadn’t moved fast enough. We should all be proud of the local teams who, from a standing start, implemented testing pathways and services, monitoring systems, the Test and Protect programme and mass vaccination within extremely short timescales never seen before.
Few of us will have lived through such rapidly changing guidance due to a growing evidence base and additional experience. We have to be forgiving of times when it seems there has been a change of minds and in this unusual context, we have to be willing to admit that what seemed the right thing to do at one stage may have to change over a relatively short time period for very good reasons.
We want to concentrate on four areas in this article that relate to decision-making in public health because our assessment is that these are the areas that require urgent ongoing action.
The problem waiting to happen – care homes
In Scotland, as of 17 January 2021, a total of 7,448 deaths were registered where COVID-19 was mentioned on the death certificate. Of these, 38% occurred in care homes. To put this into context, in 2019, 24% of all deaths in Scotland occurred in care homes. From week 12 in 2020 to week 2 in 2021 (the period since the first COVID-19 death was registered in Scotland), there were 2,350 excess deaths in care homes (18% above average), and deaths with the underlying cause of COVID-19 accounted for the majority of these excess deaths.1
A matched case-control study with data to June 2020 showed that residence in a care home was associated with a 15-fold increase in risk of severe or fatal COVID-19, after adjustment for demographic factors and underlying conditions pre-disposing for severe outcomes. Severe or fatal COVID-19 was defined by either a positive nucleic acid test followed by entry to critical care or death within 28 days or a death certificate with COVID-19 as underlying cause. Whilst residual confounding by frailty is likely to have contributed to this excess in risk for care home residents, it also reflects the spread of the epidemic in care homes.2
The COVID-19 pandemic has brought to all of our attentions the weaknesses in a care system that has been underfunded and overlooked for many years. When one of the authors of this article was first appointed as a consultant in public health medicine (CPHM) in the early 1990s, community care was in its early implementation. We were closing the large institutions and long-stay geriatric hospitals and moving many people into privately run care homes as well as to supported living and other more independent living situations.3,4 We are not defending large institutions, but even more than 20 years ago it was clear that shifting nursing home provision to the private sector led to lower pay and poorer terms and conditions for staff. These longstanding issues in how social care staff are treated was always likely to be a factor in the impact of COVID-19 in care homes. Staff often work in multiple facilities or have a number of part-time jobs. Furthermore, the challenges of caring for people with dementia, particularly when social distancing or isolation is required, makes the caring task more challenging.
The care home sector has been relatively neglected and it could be argued that the pandemic impact of unacceptable numbers of deaths was inevitable. There were many examples of staff going to work when symptomatic, having to take a day’s holiday to get tested, car sharing against the advice, all of them due to the low pay and lack of adequate sick pay and holiday pay.
The need to limit the impact of the virus in care homes has added many more burdens on these care home staff already working hard to care for a very frail group of people. The complexity and rapidly changing guidance was necessary but challenging for care home staff, and public health teams had a vital role in supporting the correct interpretation of the guidance. While we wanted to limit footfall to care homes for infection control reasons, it was quickly realised that there was no substitute for care home visits to truly understand practice and problems that needed resolution. The joint working by public health teams with care homes, the care inspectorate, nursing teams and commissioning teams has been a very positive and valuable experience that will also reap rewards in the future.
As a country, as a society, we must use this experience of COVID-19 to pay more attention to this sector. The independent review of adult social care in Scotland provides an opportunity for real improvement.
Harms beyond infection
The Scottish Government Framework for Decision Making (Scottish Government 23 April 2020) talks about the four harms that the virus causes:
- direct and tragic harm to people’s health.
- wider impact on health and social care services.
- harm to our broader way of living and society, including, for example, the negative effects of increased isolation, particularly for those living alone, and the impact on children’s well-being from closing schools.
- the wider negative impacts of the global pandemic with the enormous impact on our economy.
It is important to remember that the direct harms of COVID-19 are not limited to the physical health effects of an acute infection, but that significant proportions of individuals suffer from long-term sequelae of the infection. In February 2021, updated estimates of ‘long COVID-19’ from an ONS study reported 9.8% (95% confidence interval from 7.4% to 13.1%) of individuals with COVID-19 still had symptoms at 12 weeks.5 Estimates vary widely, partly because we are still learning about the complex multifactorial presentations known as ‘long COVID’, and definitions are not standardised across studies. Up to a third of COVID-19 patients admitted to hospital develop serious mental health consequences, including depression, anxiety, post-traumatic stress disorder, and cognitive problems. It is recognised that the mental health needs of COVID-19 patients are inextricably linked with their physical rehabilitation, requiring integration of care.6 The mental health impacts of COVID-19 and their interactions with physical health and the socioeconomic context are difficult to neatly categorise into the four harms framework, due to the complexity of experiences with infection (own, or family or friends), perception of infection risks, requirements for self-isolation, and wider social restrictions. Self-reported mental health surveillance data indicated a deterioration of mental health and well-being at the UK population level over the first national lockdown. Psychological distress, anxiety and depressive symptoms peaked in April 2020, with some recovery over the summer and autumn, but indications of renewed deterioration between October and January.7
Those who have been most affected by COVID-19 are generally those who already had the worst health outcomes before the pandemic. A matched case-control study on Scottish data to June 2020 confirmed that conditions designated as moderate risk by the NHS (including asthma, diabetes, heart disease, disabling neurological disease, kidney disease) were associated with increased risk of severe COVID-19, but also showed increased risk of severe COVID-19 for other diagnoses that are associated with frailty and poor health such as strokes and a history of falls.2 After adjustment for underlying conditions, deprivation remains an independent risk factor for severe COVID-19 outcomes.2 Compared with those in the least deprived quintile (i.e. fifth of the population), those in the most deprived quintile continue to have a higher risk of infection in waves two and three, as can be seen from local data (Figure 1).
Figure 1 NHSGGC rolling seven-day cumulative incidence of COVID-19 cases per 100,000 population, by date of notification and SIMD quintile
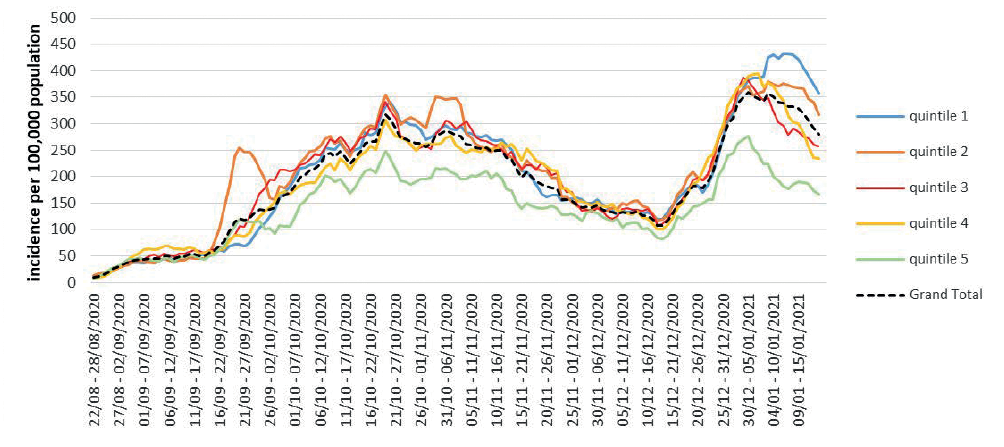
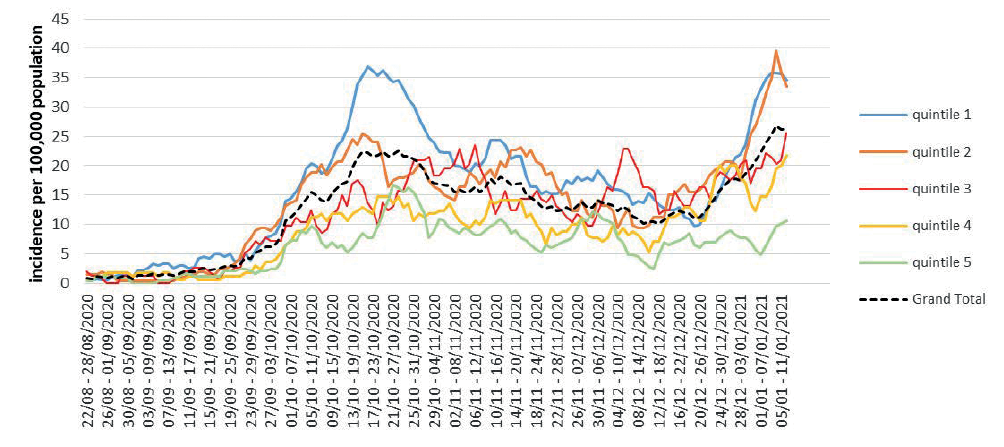
The differences between deprivation quintiles are even starker for the incidence of hospitalisations with COVID-19 (Figure 2). Data from the Scottish Intensive Care Society Audit Group additionally shows that the probability of 30-day mortality of patients admitted to intensive care units (ICUs) remains higher for patients from the most deprived compared with the least deprived quintile, though outcomes have improved for the most deprived quintile in wave 2 compared with wave 1.8Age-standardised all-cause death rates are higher in the most deprived areas compared with the least deprived areas, and this effect is even more pronounced for COVID-19. Between March and December 2020, the all-cause death rate in the most deprived quintile of the population in Scotland was 1.9times the rate in the least deprived quintile. This gap was even greater for deaths involving COVID-19, for which the rate in the most deprived quintile (208 per 100,000 population) was more than twice the rate in the least deprived quintile (94 per 100,000 population).1
Figure 2 NHSGGC rolling seven-day cumulative incidence of COVID-19 cases admitted to hospital per 100,000 population, by date of notification and SIMD quintile
It has been argued that our response to the pandemic has been too orientated to a biomedical model and that we should think much more about the interaction with non-communicable diseases (NCDs) which fuel many of our current inequalities.9The term ‘syndemic’ can be applied10to emphasise this is much more than just recognising co-morbidity because these NCDs tend to cluster within certain social groups that contribute to health inequalities. Syndemic refers to the concept of multiple diseases clustering within a population (and interacting to exacerbate outcomes), resulting from, and in turn contributing to, persistent social and economic inequalities.10 In an area like NHS Greater Glasgow and Clyde with more than its fair share of diseases such as COPD, type 2 diabetes and obesity, as well as poor mental health, particularly in areas of high deprivation, we needed a greater acceptance of this. Our decision-making did not adequately take this into account, so in future we must prioritise the prevention and management of these NCDs within all of our measures to manage the pandemic.
The pre-existing health inequalities due to poverty and deprivation have been sharply exposed during the pandemic. Even before the pandemic, improvements in life expectancy had stalled. A distinct slowdown in improvement in life expectancy and mortality rates in the UK has been observed over the last 10 years.11-13 Whilst similar changes have been reported in other high-income countries, the slowdown has been particularly marked in the UK and the USA.14 This cannot be explained as a biological ceiling to life expectancy, as other high-income countries with higher life expectancy have seen continued improvements.12,14 There is a growing body of evidence from the UK11,15-17 and from international comparisons18,19 suggesting this stalling in life expectancy is at least in part attributable to UK Government ‘austerity’ measures implemented from 2010, cuts to public services and social security which have particularly affected the most vulnerable populations. Most concerning, among the most socioeconomically deprived populations mortality rates have increased and inequalities in all-cause mortality have widened considerably since around 2012.20-22This public health emergency and inequalities crisis existed before the pandemic. The pandemic adds to the urgency of the issue if we are to reverse these trends.
Throughout the pandemic, public health has discussed and warned of the wider impacts of the pandemic. These discussions were particularly difficult when debating levels of restrictions and the balance between suppressing the virus and the harms to the economy and harms to children and young people if schools are not fully open. As directors of public health we were encouraged to concentrate on health protection harms rather than the wider three harms. This was not a comfortable position. Of course these balances and considerations are messy. While reducing mortality from the virus is a key aim of our efforts, we need to weigh up a short extension to life for people already at advanced age against potentially life-long impacts for young people, and this should be done transparently and explicitly. Otherwise public health is in danger of merging with our national sickness service and de-prioritising prevention.
Although it is difficult, it is essential that we look beyond the immediate impacts of COVID to the long-term impacts and mitigate them. David Oliver23 suggests that the narrative can all too easily become reductive and polarised, leading to false dichotomies. Applying the syndemic framework as a lens sharply brings into focus that we cannot separate health protection from the pandemic impact on jobs and mental health or social determinants. It would not help a family if the breadwinner is sick and cannot work or worse dies and it does not help a family if there are no jobs. Oliver has highlighted other dichotomies such as visiting in care homes versus discharging care home residents from hospital early on in the pandemic. He suggests that many of these issues cannot be ‘either/or’ but rather ‘both at once’ with a reweighting of priorities as contexts change. We need to take this nuanced approach. In January, with extreme pressures on acute hospitals, we needed such an approach in relation to discharges to care homes, for example the need for negative clearance tests prior to discharge from hospital to a care home.
At the same time, public health has to be willing to challenge priorities and government policy. Allyson Pollock, Professor of Public Health in Newcastle and the winner of the BMJ editors award in 2020 for ‘speaking truth to power’ said recently that an important role as a public health doctor is to question government policy.24 This means continuing to ask questions about evidence but also accepting uncertainties. She argues that, the more we discuss those uncertainties and also differences of opinion, the better understanding we have which is sometimes missing from scientific discourse. Our experience as directors of public health in Scotland was that we were able to do this in our regular meetings with the chief medical officer (CMO) and government officials. It would be interesting to debate if more of these discussions about differences of opinion could be in the public domain without risking public confidence. There is also a balance to be found between building good relationships with government officials and policy colleagues in order to influence decisions and the need at times to be overtly critical of decisions or policy. This can be a hard balance to find and requires trust and effective working with our chief executives.
The pandemic has also emphasised the need to change how health and care services work with people and communities, to a different way of working that recognises the role communities can play in improving health. We have long needed a new culture of working with communities to understand their priorities and needs and work with their strengths, but it is now needed more than ever.25,26
Strengthening this approach would encourage enhanced community support at a time of restrictions, and would also help develop more effective mechanisms for engagement and co-production with communities on the restrictions themselves.
Behaviour change
COVID-19 has emerged ‘successfully’ as a pandemic virus, with effective transmission dynamics under conditions of ‘normal’ social interactions and behaviours within and across a diverse range of cultures locally and globally. The stark patterns of COVID-19 described in the earlier sections of this paper highlight the underlying socioeconomic and demographic vulnerabilities that shape the local context of this pandemic in Scotland, and NHS Greater Glasgow and Clyde specifically. Our response to the pandemic (and attempts at control and mitigation) has been reliant on achieving immediate, dramatic, and sustained changes in behaviour to interrupt transmission.
We have learned anew lessons already known about behaviour change in health improvement: that you need clear messages; you need to motivate people appropriately; and you need legislation, supports and encouragement. Many workers need incentives to self-isolate in order to feed their families, others need support to work from home, so just telling people to do it is not enough. We need to explicitly recognise that the ability to implement advice to reduce and mitigate COVID-19 risk is strongly influenced by the social determinants of health. These influence the ability to minimise the risk of exposure to infection outside the household (e.g. employment or self-employment which does not allow home working, need to use public transport or car share, and access to high-quality green space to socialise in physically distanced fashion). They also affect the ability to isolate effectively and prevent within-household transmission (e.g. space within the household to use separate rooms and facilities, and fulfil ongoing caring responsibilities).
A review of the evidence on positive strategies for sustaining adherence to infection control behaviours by the Scientific Pandemic Influenza Group on Behaviours was published in November 202027 as part of the Scientific Advisory Group for Emergencies (SAGE) papers. It sets out key principles, many of which are based on longstanding experience and evidence from health improvement programmes.
Promoting and supporting alternatives, whenever activities that people value must be restricted, can provide an immediate alternative source of enjoyment to reduce emotional distress28,29 and may also avert unintended consequences of the restriction such as conflict with those imposing the restrictions and mixing in locations that have a higher risk of COVID-19 transmission.30 For example, when indoor socialising is restricted, it is worth proposing and facilitating physically distanced outdoor socialising, or online socialising.
Well established health behaviour evidence teaches us that positive feedback about the great efforts people are making leads to further effort,31 particularly if combined with a message that further effort is required to reach the goal,32 whereas focus on failure reduces self-confidence and lowers motivation to try.31 We should make sure to highlight the success of these efforts in helping to reduce infection rates (for example by publicising more widely the observations on reductions in contact patterns, and associated reductions in the effective reproduction rate, as published by the Scottish Government modelling group,33 as well as the further benefits if everyone can increase these efforts. The emphasis needs to be on everyone playing an important role in reducing the risk of transmission. Singling out particular sub-groups of the population (e.g. students), or attributing blame to individuals for not adhering to guidelines, is likely to lead to loss of cooperation from people with good intentions but imperfect adherence.34,35 Drawing attention to non-adherence by individuals or small groups of people is also likely to undermine social norms, as well as making people who do not belong to these groups feel less responsible for reducing the risk of transmission. Habit is one of the most powerful influences on behaviour and is cued by environments and situations where the behaviour was previously carried out.36,37Environmental changes can be implemented that will help change habits (such as ground markings in buildings, broadening pavements to allow physical distancing, and installing cycle lanes to facilitate active transport).
The evidence base for other long-term behaviour restrictions, such as diet or alcohol intake, has also shown that supporting people to plan scenarios (especially if-then plans), allows people to anticipate challenging contexts, and allows them to adhere more effectively to their intentions.38,39 In the context of COVID-19 such plans may be helpful for maintaining physical distance when seeing friends and family, or to adhere to isolation advice. Self-directed engagement with an activity to achieve the desired goal (autonomous motivation) is an important motivator and influence on behaviour. Rather than focusing on ‘obeying the rules’ (extrinsic motivation), motivation can be improved by highlighting the benefits of reducing the risk of transmission, to prevent deaths and maintain NHS capacity for treating other health problems, and to allow important activities to continue (school, work, physically distanced socialising). By focusing on risk reduction, rather than a binary approach to whether or not rules are being complied with, it is possible to support and build on efforts people are making.
Isolation of individuals infected with COVID-19, and quarantine of those known to be exposed (contacts) are the mainstay of the test and protect programme, which aims to prevent secondary and tertiary cases. To achieve this, people must recognise the relevant symptoms, come forward for testing, receive the results in a timely fashion, and be willing and able to provide the relevant information to contact tracers, and to adhere to the isolation advice. Each of these steps is essential for an effective contact tracing programme, but all investment in the early steps is to no effect unless individuals are enabled to isolated effectively.
A review of the evidence on financial incentives for self-isolation by the Scientific Pandemic Insights Group on Behaviours (SPI-B), published in October 2020 as part of the SAGE papers,40 highlighted that our understanding of adherence to self-isolation is limited by both an absence of validated measures of self-isolation, and an absence of intervention studies that evaluate the effect of different support measures for self-isolation. Survey data of the general population suggests that out of the individuals who should self-isolate (individuals self-reporting symptoms that meet the COVID-19 case definition, or with a household member with such symptoms) only a small proportion (18-25%) adhered to isolation advice and self-reported that they had not left the house in the relevant period.35,41 A small pilot survey of individuals who were already in touch with Test and Trace as index cases or contacts, had a lower bound estimate of adherence of 39%, assuming that those individuals not responding to the survey were not adhering (with a much higher self-reported adherence of 86% for cases and 89% for contacts who responded). However, approximately 70% of those reporting they were adhering to self-isolation also reported they had made ‘a final trip’ somewhere before commencing isolation, showing that they were not able to adhere to guidelines and commence isolation straight away.42
There is evidence that adherence is dependent on financial income, as well as adequate access to food and medical supplies, that mental distress affects the ability to self-isolate, and that people may continue fulfilling caring responsibilities when they should be self-isolating, thus potentially putting particularly vulnerable individuals at risk.35,41 Local authorities as well as voluntary organisations have been providing support to individuals self-isolating since the Test and Protect programme was implemented. In addition, self-isolation support grants were implemented in October, aligning with evidence from the present and previous pandemics that the ability to self-isolate for the required period of time is dependent on adequate financial support to do so.43-47 The self-isolation support grant is a £500 payment available for low-income workers who are asked to self-isolate because of coronavirus (COVID-19) and would lose income as a result. They are also available to individuals in the UK with a visa that allows them no recourse to public funds. Management information released to date for October and November shows a total of 1,856 such grants were awarded across Scotland.48 This compares with nearly 66,000 cases testing positive over October and November, more than a quarter of whom (~18,000) were in the most deprived quintile of the Scottish population.49 There should be a true partnership approach between the population and government during these difficult times.
Public health services
The final but vital aspect of our decision-making is the state of our public health teams themselves. Public health has been underfunded and undervalued for many years. The vital need for public health expertise was acknowledged early on in the pandemic but years of poor workforce planning, weak policy, lack of national leadership and fragmented responsibilities have resulted in a workforce crisis that meant even with new funding we struggled to recruit appropriately trained staff. This meant we had to find smarter ways of working especially in a large area such as Greater Glasgow and Clyde which has had the highest number of cases and outbreaks in Scotland. Excellent examples of this include our joint work with Education on contact tracing and improved joint working across a range of management and clinical teams in the NHS.
People step up in a crisis and this has never been seen more clearly than over the last year. Public health teams are more truly multidisciplinary than ever before and there are wonderful examples of people not only going the extra mile but also ensuring support for colleagues.
These excellent examples can help re-build a strong public health workforce but as a country we must not allow our public health services to weaken to the same extent ever again. Investment and support for training in public health must be a priority in future years.
References
1 National Records Scotland. Deaths involving COVID-19 Week 2: 11 Jan – 17 Jan. [Internet]. Edinburgh: National Records of Scotland [Accessed 20 January 2021]. Available from: https://www.nrscotland.gov.uk/news/2021/deaths-involving-covid-19-week-2...
2 McKeigue PM, Weir A , Bishop J et al. Rapid epidemiological analysis of comorbidities and treatments as risk factors for COVID-19 in Scotland (REACT-SCOT): a population-based case-control study. PLoS Med 2020; 17: e1003374.
3 Harrington C, Woolhandler S, Mullan J et al. Does investor ownership of nursing homes compromise the quality of care? Am J Public Health 2001; 91: 1452-5.
4 Castle NG, Engberg J. Staff turnover and quality of care in nursing homes. Med Care 2005; 43: 616-26.
5 Ayoubkhani D, Gaughan C, Jenkins J. Update on long COVID prevalence estimate, 1 February 2021 [Internet]. Newport: Office for National Statistics (ONS) [Accessed 9 April 2021]. Available from: https://www.gov.uk/government/publications/ons-update-on-long-COVID-19-p...
6 Cossette N. Meeting the mental health needs of patients hospitalised due to COVID-19: a plan for Scotland [Internet]. Edinburgh: Scottish Government, September 2020 [Accessed 9 April 2021]. Available from: https://www.gov.scot/binaries/content/documents/govscot/publications/ind...
7 Public Health England. COVID-19: mental health and wellbeing surveillance report [Internet]. London: Public Health England, 2021; updated 8 April 2021. [accessed 9 April 2021]. Available from: https://www.gov.uk/government/publications/covid-19-mental-health-and-we...
8 Scottish Intensive Care Society Audit Group. Report on COVID-19 [Internet]. Edinburgh: SICSAG; updated 7 March 2021. [Accessed 9 April 2021]. Available from: https://beta.isdscotland.org/find-publications-and-data/population-healt...
9 Horton R. Offline: COVID-19 is not a pandemic. Lancet 2020; 396: 874.
10 Singer M, Buleed N, Ostrach B et al. Syndemics and the biosocial conception of health. Lancet 2017; 389: 941-51.
11 Hiam L, Harrison D, McKee M et al. Why is life expectancy in England and Wales ‘stalling’? J Epidemiol Community Health 2018; 72: 404–8.
12 Fenton L, Minton J, Ramsay J et al. Recent adverse mortality trends in Scotland: comparison with other high-income countries. BMJ Open 2019; 9: e029936.
13 Walsh D, McCartney G, Minton J, et al. Changing mortality trends in countries and cities of the UK: a population-based trend analysis. BMJ Open 2020; 10: e038135.
14 Ho JY, Hendi AS. Recent trends in life expectancy across high income countries: retrospective observational study. BMJ 2018; 362: k2562.
15 Green M, Dorling D, Minton J. The geography of a rapid rise in elderly mortality in England and Wales, 2014-15. Health Place 2017; 44: 77–85.
16 Loopstra R, McKee M, Katikireddi SV et al. Austerity and old-age mortality in England: a longitudinal cross-local area analysis, 2007-2013. J R Soc Med 2016; 109: 109–16.
17 Stuckler D, Reeves A, Loopstra R et al. Austerity and health: the impact in the UK and Europe. Eur J Public Health 2017; 27: 18-21.
18 Rajmil L, Fernández de Sanmamed M-J. Austerity policies and mortality rates in European countries, 2011-2015. Am J Public Health 2019; 109: 768–70.
19 Toffolutti V, Suhrcke M. Does austerity really kill? Econ Hum Biol 2019; 33: 211–23.
20 Public Health England. Recent trends in mortality in England: review and data packs. [Internet]. London: Public Health England 11 December 2018 [Accessed 4 February 2021]. Available from: https://www.gov.uk/government/publications/recent-trends-in-mortality-in...
21 Fenton L, Wyper GM, McCartney G et al. Socioeconomic inequality in recent adverse all-cause mortality trends in Scotland. J Epidemiol Community Health 2019; 73: 971–4.
22 Scottish Government. Long-term monitoring of inequalities. December 2018 report. [Internet]. Edinburgh: Scottish Government 11 December 2018. [Accessed 4 February 2021]. Available from: https://www.gov.scot/publications/long-term-monitoring-health-inequaliti...
23 Oliver D. David Oliver: The false dichotomies in pandemic commentary. BMJ 2021; 372: m4937.
24 Mahase E. “In the 1980s NHS there wasn’t today’s climate of fear around speaking out”–Allyson Pollock. BMJ 2021; 372: m4930.
25 Inspiring Scotland. Link up: transforming relationships. Annual publication 2019-20. Edinburgh: Inspiring Scotland 2020.
26 Scottish Community Development Centre. SCDC Statement on the COVID-19 crisis. [Internet]. Glasgow: Scottish Community Development Centre. Available from: https://www.scdc.org.uk/news/article/2020/3/19/scdc-statement-on-the-cov...
27 SPI-B. Increasing adherence to COVID-19 preventative behaviours among young people [Internet]. 6 November 2020a. [Accessed 4 February 2021]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploa...
28 Kwasnicka D, Dombrowski SU, White M et al. Theoretical explanations for maintenance of behaviour change: a systematic review of behaviour theories. Health Psychol Rev 2016; 10: 277-96.
29 Patey AM, Hurt CS, Grimshaw JM et al. Changing behaviour ‘more or less’ – do theories of behaviour inform strategies for implementation and de-implementation? A critical interpretive synthesis. Implementation Sci 2018; 13: 134.
30 Polivy J. The effects of behavioral inhibition: integrating internal cues, cognition, behavior, and affect. Psychological Inquiry 1998; 9: 181-204.
31 Strecher VJ, DeVellis BM, Becker MH et al. The role of self-efficacy in achieving health behavior change. Health Educ Q 1986; 13: 73-92.
32 Fishbach A, Eyal T, Finkelstein SR. How positive and negative feedback motivate goal pursuit. Soc Personal Psychol Compass 2010; 48: 17-5301751
33 Scottish Government. Coronavirus (COVID-19): modelling the epidemic in Scotland (issue no.35). [Internet]. Edinburgh: Scottish Government; 21 January 2021 [Accessed 4 February 2021]. Available from: https://www.gov.scot/publications/coronavirus-covid-19-modelling-epidemi...
34 Bonell C, Jamal F, Melendez-Torres GJ et al. ‘Dark logic’: theorising the harmful consequences of public health interventions. J Epidemiol Community Health 2015; 69: 95-8.
35 Smith LE, Amlôt R, Lambert H et al. Factors associated with adherence to self-isolation and lockdown measures in the UK: a cross-sectional survey. Public Health 2020; 187: 41-52.
36 Hagger MS. Habit and physical activity: theoretical advances, practical implications, and agenda for future research. Psychol Sport Exerc 2019; 42.
37 Gardner B, Lally P, Wardle J. Making health habitual: the psychology of ‘habit-formation’ and general practice. Br J Gen Pract 2012; 62: 664-6.
38 Lawlor ER, Hughes CA, Duschinsky R et al. Cognitive and behavioural strategies employed to overcome “lapses” and prevent “relapse” among weight-loss maintainers and regainers: a qualitative study. Clin Obes 2020; 10: e12395.
39 Mason F, Farley A, Pallan M et al. Effectiveness of a brief behavioural intervention to prevent weight gain over the Christmas holiday period: randomised controlled trial. BMJ 2018; 363: k4867.
40 SPI-B. Impact of financial and other targeted support on rates of self-isolation or quarantine [Internet]. 9 October 2020b. [Accessed 4 February 2021]. Available from: https://www.gov.uk/government/publications/spi-b-impact-of-financial-and...
41 Smith LE, Potts HW, Amlôt R et al. Adherence to the test, trace and isolate system: results from a time series of 21 nationally representative surveys in the UK (the COVID-19 Rapid Survey of Adherence to Interventions and Responses [CORSAIR] study). BMJ (submitted) NHS Test and Trace. Isolation compliance survey pilot. 2020.
42 NHS Test and Trace, 2020 SPI-B. The impact of financial and other targeted support on rates of self-isolation or quarantine [Internet]. 16 September 2020. [Accessed 9 April 2021]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploa...
43 Rothstein MA, Talbott MK. Encouraging compliance with quarantine: a proposal to provide job security and income replacement. Am J Public Health 2007; 97 Suppl 1: S49-56.
44 Blake KD, Blendon RJ, Viswanath K. Employment and compliance with pandemic influenza mitigation recommendations. Emer Infect Dis 2010; 16: 212-8.
45 Kavanagh AM, Mason KE, Bentley RJ et al. Leave entitlements, time off work and the household financial impacts of quarantine compliance during an H1N1 outbreak. BMC Infect Dis 2012; 12: 311.
46 Kumar S, Quinn SC, Kevin HK et al. The impact of workplace policies and other social factors on self-reported influenza-like illness incidence during the 2009 H1N1 pandemic. Am J Public Health 2012; 102: 134-40.
47 Bodas M, Peleg K. Self-isolation compliance in the COVID-19 era influenced by compensation: findings from a recent survey in Israel. Health Aff (Millwood) 2020; 39: 936-41.
48 Scottish Government. Scottish Welfare Fund, Self-Isolation Support Grant and discretionary housing payments: monthly data. Management information on Scottish Welfare Fund and Self-Isolation Support Grants and Official Statistics on Discretionary Housing Payments to November 2020. [Internet]. Edinburgh: Scottish Government; 12 January 2021, updated 9 February 2021 [Accessed 11 February 2021]. Available from: https://www.gov.scot/publications/swf-monthly-management-information/#:~...
49 Public Health Scotland. Daily COVID-19 Cases in Scotland. Daily cases trends by deprivation. [Internet]. Edinburgh: Public Health Scotland [Accessed 4 February 2021]. Available from: https://www.opendata.nhs.scot/dataset/covid-19-in-scotland