Pandemics are not new
The issues in this pandemic resemble those in virtually every other pandemic. For example the ‘Russian pandemic’ of the 1890s was the sixth of the nineteenth century in the UK, whereas the twentieth century saw only three. Again we think it originated in China and spread through Europe. The observed case fatality rate was lower than in the infamous 1918 pandemic. But it interrupted the decline in communicable disease which characterised the nineteenth century following sanitary reforms. It caused mass illness, disrupted the economy, suspended Parliament and the postal service,1,2 and led the young Winston Churchill to write a poem.3Transmission was intensified by the absence of sick pay and failure to stay at home as advised, for fear of losing employment.
Experience of COVID-19 in Scotland
Many of these issues are relevant today. But every pandemic is different – in severity, those most responsible for transmission, and those affected. COVID-19 has seriously affected the elderly and those with certain underlying diseases, but been milder in children and those under 40. Though children spread influenza most, people between 20 and 40 are greater spreaders of COVID-19.
Figure 1 shows the confirmed cases of COVID-19 in Scotland from 1 March 2020 to March 2021. Figures 2, 3 and 4 divide this into three phases and identify key events along the way. It was on 30 January that WHO declared COVID-19 a public health emergency of international concern (PHEIC). As February progressed, it became clear that Northern Italy was the epicentre of the pandemic in Europe caused, we think, by growing business links with the manufacturing sector in China. The next significant event was the ‘Nike Conference’ in Edinburgh on 26 and 27 February, attended by delegates from several countries, the first recorded evidence of international spread through a conference in the UK. More importantly this conference heralded the role of whole genome sequencing in mapping and understanding transmission. Combined phylogenetic and epidemiological analysis showed that COVID-19 arrived in Scotland on hundreds of occasions during February and March 2020, mainly from Italy and Spain.4
Figure 1 Confirmed COVID-19 cases in Scotland, March 2020-March 2021
Figure 2 Confirmed COVID-19 cases in Scotland during the first wave and key events, February - July 2020
Figure 3 Confirmed COVID-19 cases in Scotland during the second wave and key events, August – November 2020
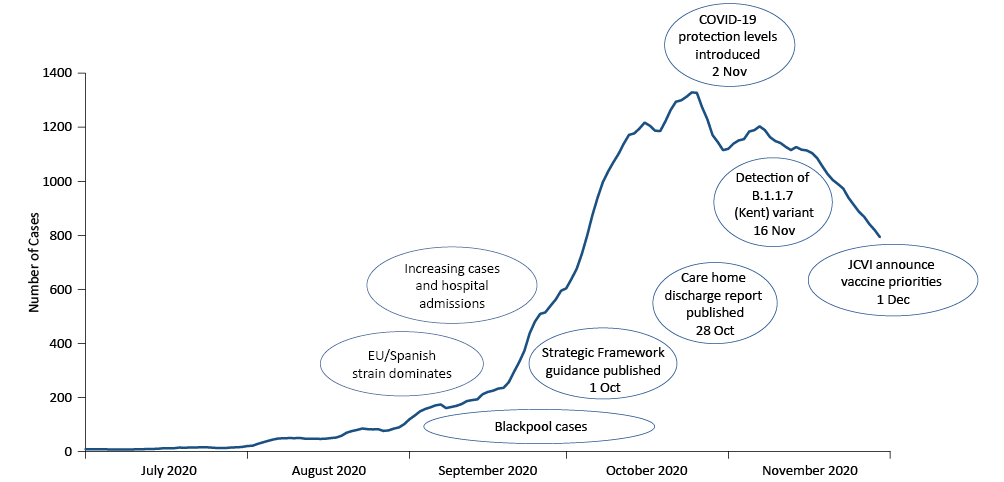
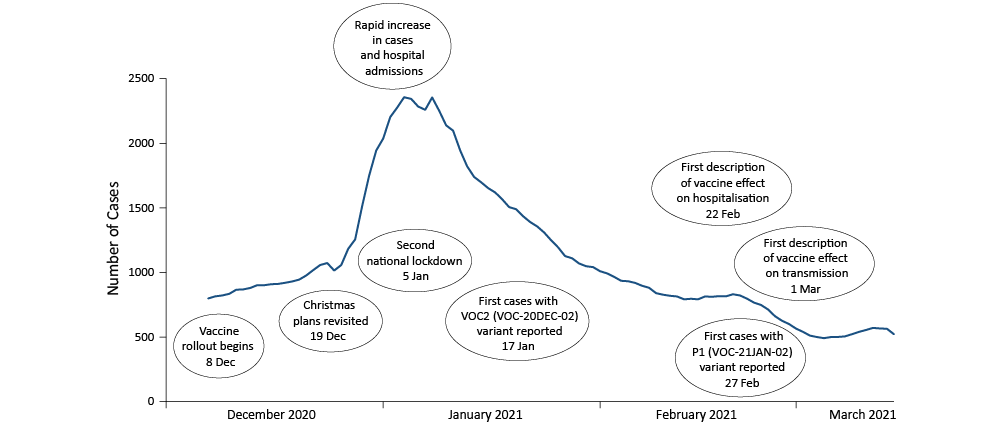
Figure 4 Confirmed COVID-19 cases in Scotland during the second wave and key events, December 2020 – March 2021
On 1 March we identified the first Scottish case, who had returned home from Italy and became unwell in the last days of February. On 11 March WHO declared COVID-19 a pandemic. The first death in Scotland occurred on 13 March. On 23 March the first UK lockdown required everyone to stay at home, and led to the mass closure of many facilities and activities across the UK. We soon saw the peak of case detection in the first wave, followed by the peak of deaths in care homes on 1 May. Cases steadily declined from then till the end of the first wave at the start of July. During this period PHS played a major role in the national response including: rapid diagnostic testing (‘drive through’ and at home); development of triage services and assessment pathways led by GPs in partnership with infectious diseases teams; planned expansion of critical care; shielding and support for vulnerable populations, including homeless people and prisoners; port health measures established before the first case in Scotland; and systematic reviews to inform all aspects of public health policy.
In the second wave starting in August, the Spanish or 20A.EU1 variant dominated; and there were many more hospital admissions and cases than in the first wave. As a result of relaxing lockdown, ‘staycations’ became popular, notably from Scotland to Blackpool. The first case we associated with Blackpool was on 14 September. Over the next six weeks, there were 747 cases linked to people from Scotland visiting Blackpool. So on 14 October we cautioned against non-essential travel to Blackpool. Whole genome sequencing enabled us to identify several strains circulating in Blackpool; and link those to subsequent increases in Scotland – in cases and in variants.
On 1 October Scottish Government published its first Strategic Framework, including phased plans to restore greater normality to daily life. On 20 October they followed with a report examining how care homes had coped with the first wave and making key recommendations to reduce deaths from COVID-19 in residents including: testing residents; when to discharge them from hospital; the support needed for this; and other measures to prevent infection in homes.5
On 2 November Scottish Government introduced protection levels across Scotland, which linked public health measures to local levels of detected COVID-19 and other evidence of transmission. On 16 November a variant was identified that later became the Kent or B.1.1.7 variant. This rapidly became prevalent, first in England, then in Scotland, and later in US, Mexico, Europe and across the globe. This appeared more transmissible than the Spanish strain, and later proved to increase case hospitalisation rates.
On 1 December the UK Joint Committee on Vaccination and Immunisation announced priorities for COVID-19 vaccines in the light of British approval for the Pfizer and Astra Zeneca vaccines: vaccination started with older age groups and those with underlying conditions. Though rollout across the UK began on 8 December, it did not start in earnest till after Christmas. In the meantime, cases and hospital admissions began to accelerate, possibly in response to the prospect of fewer restrictions over Christmas. So the second national lockdown was launched on 5 January.
On 17 January we first detected the South African or B.1.351 variant, potentially more resistant to the current vaccines. This reinforced the importance of whole genome sequencing in identifying new variants, in particular those which were more transmissible, more likely to evade the immune response, or associated with more severe disease. On 27 February, we recognised the Brazilian or P1 variant, which is of particular concern because protection against earlier strains of COVID-19 may not be effective against P1, as shown by an upsurge in cases in Brazil.
More reassuringly, on 22 February a team based in Scotland reported that vaccination had reduced hospitalisation by 90% – the welcome first evidence that the vaccine was working.6 On 21 March another team based in Scotland reported that vaccinated healthcare workers were 55% less likely than unvaccinated workers to transmit COVID-19 to people in the same household.7
Key issues in responding to COVID-19 in Scotland
Figure 5 shows how the 7-day moving average of cases increases with deprivation. The most deprived areas – those in the most deprived fifth of the population (also known as the most deprived quintile), experienced 50% more cases than those in the least deprived fifth; and this difference was more marked in the second wave. Figure 6 shows the most deprived areas also suffered twice as many deaths as the least deprived, in both first and second waves. Thus the pandemic has reinforced the need to address inequity across Scotland.
Figure 5 inequalities in COVID cases
Figure 6 inequalities in COVID deaths
Early in the pandemic, fearing that COVID-19 would worsen the existing gross differences in morbidity and mortality, an augmented team from PHS undertook a health impact assessment to identify the range of potential harms that PHS and Scottish Government needed to mitigate,8 ideally before initial lockdown. As well as the direct effects of COVID-19, these harms included a wide range of adverse effects of the measures designed to counter COVID-19, notably isolation at home, working from home where possible, bans on social gatherings, restrictions on travel, closure of educational facilities and inessential workplaces, and limiting contact with special populations, for example in care homes and prisons. Those adverse effects included disruption of economic activity (especially loss of jobs and income), education at all levels, essential services, exercise, family life, health-seeking behaviour, psychosocial well-being, social cohesion, social order, and transport. The PHS team also analysed the social groups most likely to suffer from each of these effects; the likely impacts on each of those groups; and potential mitigations and mitigators.8
In response to this assessment, PHS established a social and systems recovery group, which produced advice and guidance on recovery.9 While we develop and refine appropriate analytical frameworks, we continue to add data to existing models, as Figure 5 and 6 exemplify. Conscious of the danger of parochialism, we shall also seek to exploit developing international comparisons, for example that published recently by Haldane et al on health systems resilience.10 Though it is too early to evaluate the national, regional and local management of the pandemic by the multitude of existing and pandemic-generated organisations across Scotland, we can already see evidence of unprecedented responses throughout the nation.
To take one specific issue, we ask: what has whole genome sequencing added? Figure 7 shows that in the first wave, there was considerable variation, associated with multiple importations of variants from Europe and beyond into Scotland. But that variation decreased in the second wave, and different variants predominated. From mid-August the common variant here was the 20A EU1, also most common in Europe, presumably reflecting visits to Spain, Italy and other holiday destinations. In 2021 the B.1.1.7 rapidly established itself and is now the predominant variant, causing 80% to 90% of cases. Fortunately this variant exhibits a distinctive feature called ‘S gene dropout’, which enables ‘polymerase chain reaction’ (PCR) tests to detect the change in the spike protein that rendered the S gene negative. This gave us a good marker to follow the transmission of this variant across Scotland at a time when only about 5% of isolates underwent whole genome sequencing.
Figure 7 Diversity of the SARS-CoV-2 sequenced in Scotland during the first and second waves
Lessons from COVID-19
The pandemic has strengthened the role of whole genome sequencing in monitoring the transmission and mutation of COVID-19. This helps to assess the effectiveness of vaccines and change them to protect us against new variants. So Scottish Government are now committed to invest in whole genome sequencing: both in the short term for COVID-19; and in the longer term for other pathogens. The second legacy is the opportunity to redesign many of our health and social care services. We have seen major changes in the way we use digital media; and in the way people access care services. It has also encouraged better use of our estate. For example, can more people work from home? So do we need such large workplaces? Will this affect our carbon footprint in future? The third and most exciting legacy is the scope for greater integration. Many groups who had not previously worked together have joined forces to address common issues. We must ensure the resulting partnerships endure and flourish; and explore ways of building more coherent strategies and programmes for the benefit of the Scottish people.
Even more challenging is the need to resolve the major inequalities exacerbated by COVID-19. We need to stimulate the economy to replace the employment lost through COVID, and to become more inclusive. We also need to revitalise and streamline education, not least to make up for a lost year. We need to remind people that the NHS is open and striving to eliminate perceived barriers. We also need to look at what we can do to promote recovery in the social sector.
There is a rare opportunity to ameliorate Julian Tudor Hart’s ‘inverse care law’,11 primarily by targeting services on those most in need, but also by explicitly monitoring the impact of our campaign to overcome disadvantage due to social position and ethnicity. We must aim to ‘build back fairer’ as the pandemic recedes. In particular we need to pursue Public Health Scotland’s four key priorities: poverty; children and young people; place and community; and mental health and well-being. The last requires us to find ways of meeting needs aggravated by this pandemic.12 As there is evidence that the pandemic has also undermined diet and exercise, there is a case for making that our fifth key area, and seeking to reclaim pre-pandemic levels of nutrition and fitness. 
Acknowledgments
I thank the COVID-19 Real-time Epidemiology Team within Public Health Scotland especially Dr Jim McMenamin (Consultant in Health Protection) who directed most of the instant PHS response, Dr Kimberly Marsh (Consultant Scientist) and Dr Gerard McCartney (Consultant in Public Health). I acknowledge the contribution of the editorial team and the two assiduous referees.
References
1 Hardy A. Cholera, quarantine and the English preventive system 1850-1895. Med Hist 1993; 37: 250-69.
2 Honigsbaum M. The ‘Russian’ influenza in the UK: lessons learned; opportunities missed. Vaccine 2011; 29 suppl 2: B11-B15.
3 Nicoll A, Mori K, Tashiro M. Churchill’s flu poem. BMJ 2008; 337 :a2890.
4 da Silva Filipe A, Shepherd JG, Williams T et al. Genomic epidemiology reveals multiple introductions of SARS-CoV-2 from mainland Europe into Scotland. Nat Microbiol 2021; 6: 112-22.
5 Burton JK, Bayne G, Evans G et al, Evolution and effects of COVID-19 outbreaks in care homes: a population analysis in 189 care homes in one geographical region of the UK. Lancet Healthy Longev 2020; 1: e21-e31.
6 Vasileiou E, Simpson CR, Shi T et al. Interim findings from first-dose mass COVID-19 vaccination roll-out and COVID-19 hospital admissions in Scotland: a national prospective cohort study. Lancet 2021; 397: 1646-57.
7 Shah ASV, Gribben C, Bishop J et al. Effect of vaccination on transmission of COVID-19: an observational study in healthcare workers and their households. medRxiv 2021.
8 Douglas M, Katikireddi SV, Taulbaut M et al. Mitigating the wider health effects of COVID-19 pandemic response. BMJ 2020; 369: m1557.
9 Oldcorn E on behalf of Social and Systems Recovery Inclusion Health Group. Inclusion health principles and practice: an equalities and human rights approach to social and systems recovery and mitigating the impact of COVID-19 for marginalised and excluded people. Edinburgh: Public Health Scotland; 2020.
10 Haldane V, De Foo C, Abdalla SM et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med 2021.
11 Hart JT. The inverse care law. Lancet 1971; 1: 405-12.
12 Niedzwiedz CL, Green MJ, Benzeval M et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of UK Household Longitudinal Study. J Epidemiol Community Health 2021; 75: 224-31.
