Every scientific paper should provide the minimum information required to enable a complete understanding of the study findings. Initially, the need for reporting standards for systematic reviews and randomised controlled trials was needed in view of numerous such articles published in the latter part of the last century that did not conform to any such standards. More often than not, such standards were set by committees of interested scientists, rather than by a formal, dedicated and rigorous process. The need for such guidelines on reporting standards to be developed and periodically updated and re-evaluated for different types of scientific articles (from case reports to systematic reviews) led to the establishment of the Enhancing the Quality and Transparency of Health Research (EQUATOR) network, which was tasked with formally prescribing such minimum reporting standards.1,2
Presently, the EQUATOR network prescribes more than 400 different types of reporting standards. In this editorial, we briefly discuss the salient features of reporting standards for those types of articles generally published in this journal, viz. case reports (CARE – Case Report),3 observational studies (STROBE – Strengthening The Reporting Of Observational Studies),4 clinical trials (including their protocols; CONSORT – Consolidated Standards of Reporting Trials,5 SPIRIT – Standard Protocol Items: Recommendations for Interventional Trials6), systematic reviews (PRISMA – Preferred Reporting Items for Systematic Reviews and Meta-analyses7), practice guidelines (AGREE – Appraisal of Guidelines, Research and Evaluation8) and qualitative research.9
Some overarching principles span most of these guidelines. The title should clearly mention the type of study. For original research articles (observational or clinical trials), preferably the setting and population should also be indicated. In the former, it is important to distinguish prospective studies from retrospective ones by mentioning this in the title. Preferably, clinical trials and systematic reviews should have a pre-published protocol, clearly delineating primary objectives from secondary ones. Protocols may need amendment during the progress of the study; these amendments should clearly be justified, delineated and available to view. Clinical trial registration is now considered mandatory, and sites where trials are registered should provide the trial protocol (and its amendments) for review.
Owing to the emerging problem of redundant systematic reviews, pre-registration of systematic reviews is highly recommended. This can be carried out under the Cochrane library if the Cochrane group has commissioned the said systematic review, or under the International Prospective Register of Systematic Reviews (PROSPERO).10 Since adequate understanding of any study relies on whether the study was suitably powered to detect an effect/difference between groups, original research articles should detail how the sample size was calculated. Ethical aspects of any published research that includes patients as subjects should be detailed in the manuscript. For a case report, it is considered best practice to seek informed consent to publish, which necessitates that the patient in question has read and approved the case report, and the report is suitably anonymised. For observational studies and clinical trials, ethical committee approval in line with local regulations is mandatory. The ethics committee may waive informed consent for retrospective retrieval of data from anonymised medical records.
Clinical trials (and systematic reviews of clinical trials) should detail methodological aspects, including randomisation, allocation concealment and blinding, and also attempt to study how much the planned blinding was successful. Subject selection should be preferably delineated in the form of a flowchart, detailing how many were screened, how many excluded (with justification for the exclusions), how many agreed to participate in a study and how many completed the study duration (for studies with a follow-up component). Patients, interventions (and comparator) and outcomes need to be clearly defined.
The results should separately describe the primary and secondary outcomes, and consider the effect of potential confounding factors for the analyses. Wherever possible, quantitative estimates of effect should be presented, along with their confidence intervals, rather than just the significance level. The findings should be discussed in context, taking care not to overstate the findings beyond a reasonable limit, and declaring transparently potential limitations of the study. Sources for the funding of a study should also be transparently declared. Further, the involvement of the funder in analysing the data and writing the manuscript, if any, should also be declared.
For systematic reviews, it is particularly recommended to include a detailed search strategy for at least one database. Also, assessment of heterogeneity of included studies, and quality assessment of studies, including that of the risk of bias, are mandatory for systematic reviews. An emerging consideration for clinical trials is the inclusion of patient reported outcomes (PROs), and minimum standards for such trials reporting PROs have been recently prescribed (the CONSORT PRO extension).11 PROs used in clinical trials should be validated, the use of PROs as primary or secondary trial outcomes should be clearly identified, the individual PRO should be detailed in the study, and their use should only be carried out in a population where they have been shown to be valid.
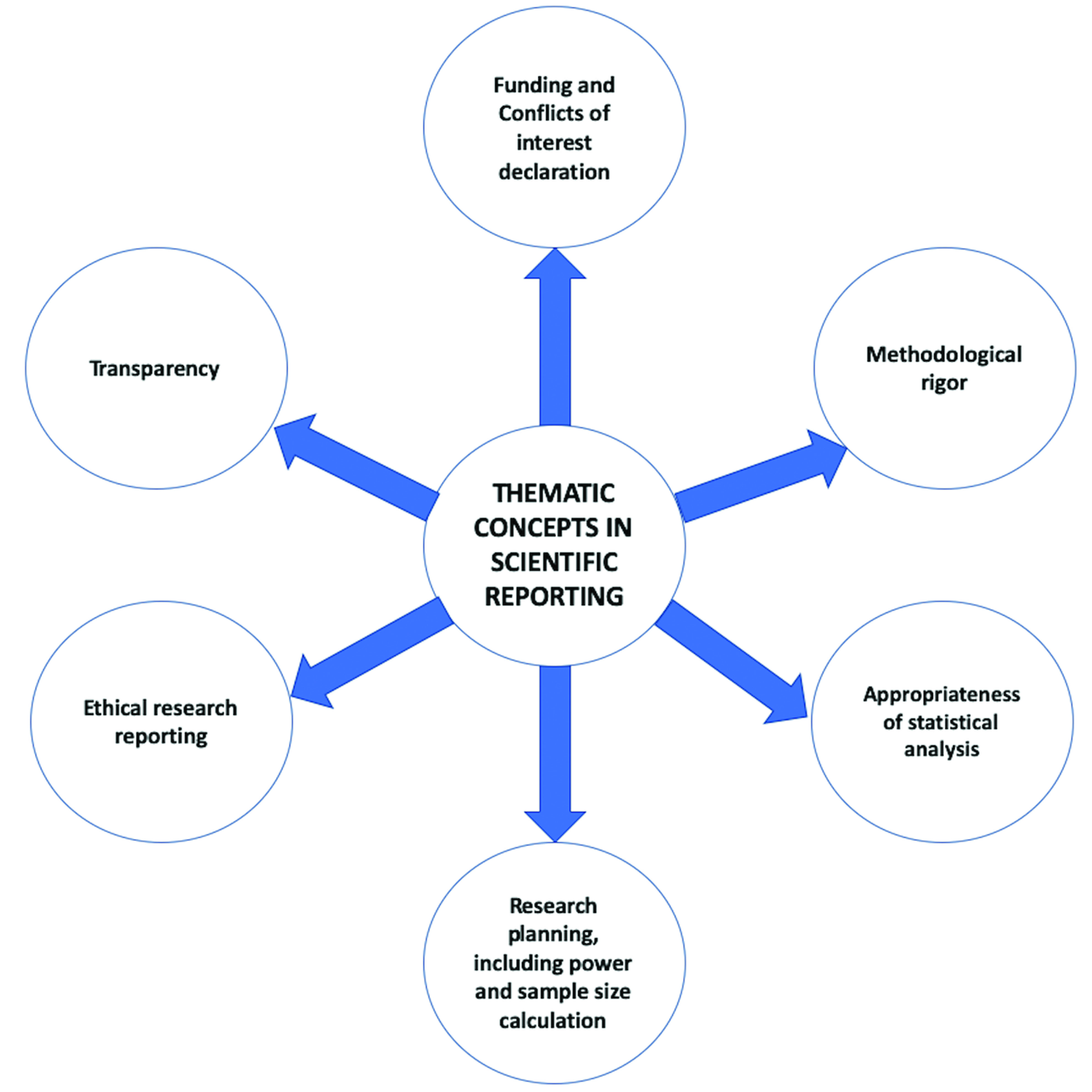
Qualitative research studies should detail the methodology used to arrive at the qualitative synthesis and analysis of data. Reporting standards for guideline development (AGREE II12) emphasise the need to detail methodological rigor in the development of the said guideline, to have clear presentation of recommendations and to declare any potential conflicts of interest for the authors.3–7,9,11,12 Figure 1 represents the thematic concepts in appropriate research reporting.
Figure 1 Thematic concepts in scientific reporting
Despite published reporting standards, there remains a need to enhance the uptake of these standards amongst authors and journals. An analysis of nearly 70 haematology journals listed in the Web of Science revealed a deficit in adhering to reporting standards in nearly half of these journals.13 Similarly, another analysis of more than 100 papers published in 2012 in reputed journals on diagnostic accuracy of tests revealed a mean of only 10.1 items being fulfilled on the recommended reporting standards checklist of 21 items.14
Courses on scientific writing should introduce such reporting standards during the training of prospective researchers. Journals, their editors and reviewers should attempt to ensure adherence to reporting standards in an attempt to enhance quality of reported research and make data across multiple studies more amenable for quantitative synthesis in systematic reviews. With the increase in numbers of review articles, there may also be a need to mandate formal reporting standards for narrative reviews as well, detailing literature searches, preferably across multiple databases, to complement already existing recommendations.15 Reporting standards also need to be updated regularly. For example, the PRISMA guidelines do not mandate literature searches across multiple databases, nor do they mandate searches across conference abstracts and clinical trial databases to identify unpublished studies.7 Therefore, future iterations of the PRISMA guidelines may take these aspects into consideration.10 Akin to the evolution in science, reporting guidelines will inevitably evolve to continually recommend the current best practices in scientific reporting.
References
1 Simera I, Altman DG, Moher D et al. Guidelines for Reporting Health Research: the EQUATOR Network’s survey of guideline authors. PLoS Med 2008; 5: e139.
2 Moher D, Liberati A, Tetzlaff J et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009; 339: b2535.
3 Gagnier JJ, Kienle G, Altman DG et al. The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol 2014; 67: 46–51.
4 von Elm E, Altman DG, Egger M et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 2007; 4: e296.
5 Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 2010; 152: 726–32.
6 Chan AW, Tetzlaff JM, Altman DG et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013; 158: 200–7.
7 Moher D, Liberati A, Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097.
8 Brouwers MC, Kho ME, Browman GP et al. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ 2010; 182: E839–42.
9 O’Brien BC, Harris IB, Beckman TJ et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014; 89: 1245–51.
10 Misra DP, Ravindran V, Agarwal V. Integrity of authorship and peer review practices: challenges and opportunities for improvement. J Korean Med Sci 2018; 33: 14.
11 Calvert M, Blazeby J, Altman DG et al. Reporting of patient-reported outcomes in randomized trials: the CONSORT PRO extension. JAMA 2013; 309: 814–22.
12 Brouwers MC, Kerkvliet K, Spithoff K. The AGREE Reporting Checklist: a tool to improve reporting of clinical practice guidelines. BMJ 2016; 352: i1152.
13 Wayant C, Smith C, Sims M et al. Hematology journals do not sufficiently adhere to reporting guidelines: a systematic review. J Thromb Haemost 2017; 15: 608–17.
14 Korevaar DA, Cohen JF, Hooft L et al. Literature survey of high-impact journals revealed reporting weaknesses in abstracts of diagnostic accuracy studies. J Clin Epidemiol 2015; 68: 708–15.
15 Gasparyan AY, Ayvazyan L, Blackmore H et al. Writing a narrative biomedical review: considerations for authors, peer reviewers, and editors. Rheumatol Int 2011; 31: 1409–17.