Introduction
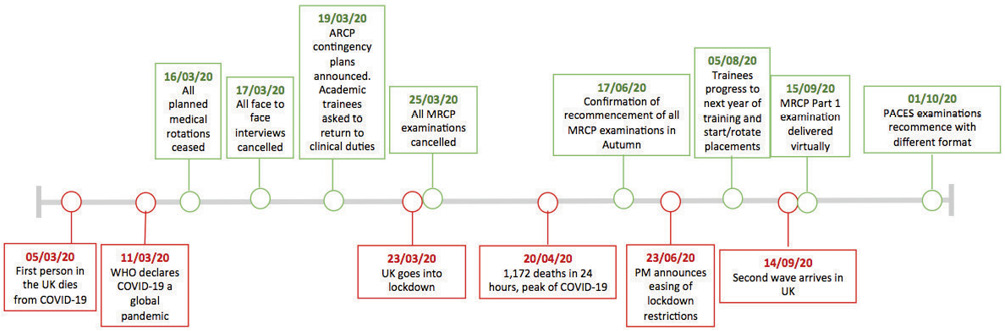
In the weeks leading up to the first peak of COVID-19 infection in the UK, drastic changes in the management of the National Health Service (NHS) machinery had to be made in order to cope with the rising surge of cases and to focus on the priority of battling the virus and preserving life. In this endeavour, healthcare workers from all sectors of the NHS had to work together to reduce morbidity and mortality from this new disease. The pandemic has necessitated a dramatic restructuring of the workforce and medical education had to rapidly transform as a consequence. Figure 1 outlines the timeline of the first wave of COVID-19 and its impact on training, This review discusses these changes and the implications on internal medicine training in the UK.
Figure 1 Timeline of the first wave of COVID-19 in the UK and its impact on training
Medical workforce
During the first peak of the COVID-19 pandemic in the UK, medical workforce augmentation was paramount to ensure the NHS could safely manage the influx of COVID-19 patients. The Academy and UK Medical Royal Colleges and Faculties issued a statement on 27 March 2020 recognising that clinicians required flexibility to be able to work outside their normal scope of practice, in order to provide the best care for patients.1 Trainee doctors from various specialties, such as general surgeons, radiologists and dermatologists, were redeployed to COVID-19 wards2,3 and academic trainees were asked to return to clinical duties. As they often worked outside of their comfort zones, redeployed staff required training to safely care for medical patients. Innovative cross-skilling training courses, which combined face-to-face and virtual elements, were designed and delivered to support trainees feel more confident and prepared in treating acutely unwell patients.4
The General Medical Council (GMC) permitted temporary registration to additional doctors under emergency legislation, to allow those who were not currently practicing to return and help with the COVID-19 pandemic.5 In addition, final year medical students were granted early graduation due to the feared disruption of clinical examinations and subsequent delay in their graduation.5 For the first time, final year medical students were offered the chance to start their foundation training early as ‘interim foundation doctors’ and more than 2000 medical students signed up to help the NHS.6 Although many trainees found the expedited start useful as a transition period before their official start, others have expressed concerns about the wellbeing of these students who may have started without a break after medical school.7
Training
As part of the national plan to combat COVID-19, important and drastic steps have been taken within healthcare in order to minimise transmission rates and to allow all efforts to focus on tackling the disease. This has been achieved in part by reducing or cancelling all ‘non-urgent’ or ‘elective’ work. This has led to fewer opportunities for trainees to see and learn from elective inpatient cases and undertake elective procedures such as endoscopy or bronchoscopy. Furthermore, there was a significant reduction in the number of outpatient clinics, and essential clinics were largely converted to ‘tele-clinics’ or ‘non-face-to-face’ encounters. The number of clinicians allowed when essential ‘face-to-face’ clinics were undertaken was limited to prevent unnecessary exposure of patients to more healthcare workers and to maintain social distancing. Telephone clinics were new for all and learning for trainees through these encounters was not without challenges. With the required minimum number of clinic attendances for internal medicine trainees (IMTs) being 80 by the end of the 3-year programme,8 there was significant concern amongst trainees about their ability to meet this requirement. In response to this predicament, the Joint Royal Colleges of Physicians Training Board (JRCPTB) acknowledged the impact of COVID-19 on outpatient opportunities and in September 2020, the clinic attendance requirement was amended, making it preferable but not mandated.9 Lastly, there was a significant reduction, deferral or cancellation of many non-urgent educational meetings, conferences and teaching. Undoubtedly, these changes had a significant impact on medical training not only through reduction in training opportunities available to trainees, but also through disruptions to the training programme.
The disruption to training has included deferring or cancelling of planned progression through clinical rotations as safe departmental inductions and appropriate supervisions for all trainees could not be secured. This meant that many trainees missed the chance to rotate to a specialty of interest and to develop certain curriculum competencies, particularly for those in their final year of core training.
Many Royal Colleges and Licensing Bodies had to defer or cancel examinations, sometimes at short notice. In March 2020, the Royal Colleges of Physicians (RCP) had to cancel all MRCP examinations in the UK. The planned change in examination format of the MRCP Part Two Clinical Examination (Practical Assessment of Clinical Examination Skills [PACES]) scheduled to be implemented in 2020 had to be delayed until 2022. Such examinations, which are designed to test trainee doctors’ clinical knowledge and skills and are a prerequisite for entering higher specialty training in the UK,10 often take trainees many months to adequately prepare for. From the trainee perspective, planned examinations are time precious as the examination diets are only held three times in any academic year, and therefore deferral or cancellation of such an examination puts a trainee’s progression in jeopardy as well as perpetuating uncertainty as to when to resume independent revision.
In June 2020, the MRCP(UK) confirmed the re-commencement of all parts of the examinations in Autumn 2020 [MRCP(UK) 2020]. In September 2020, and for the first time in the history of MRCP examinations, the MRCP Part One examination was delivered online for candidates in certain geographical locations [MRCP(UK), 2020]. Whilst this change ensured candidates remained socially distant and avoided the need or risk of travelling potentially long distances to undertake this examination, there were valid concerns regarding the reliability of internet connection and ensuring robust standards of invigilation were met. The MRCP PACES examination also made adjustments for patients, candidates and clinicians’ safety whilst maintaining the validity and reliability of the examination. Such adjustments included addition of extra time between clinical encounter stations to encompass donning and doffing of Personal Protective Equipment (PPE) and using remote surrogates and examiners in the communication stations [MRCP(UK) 2020]. The impact of these changes on candidate performance and examination reliability and validity is not yet known.
Due to these disruptions to training, the Annual Review of Competency Progression (ARCP) requirements for trainees were eased. New ARCP allowances have been made to ensure trainees who missed training opportunities or did not acquire certain competencies due to the COVID-19 pandemic were not unfairly discriminated against and to allow them to complete or progress in their training programmes.
Teaching
The pandemic has had significant repercussions on teaching methods used to deliver medical education in the UK. For some UK doctors in training, there was a near-total focus on service and care provision for patients rather than learning through scheduled teaching.
Given the government’s recommendations to cancel large gatherings and limit in-person interactions, most pre-pandemic hospital teaching, such as case conferences, multidisciplinary meetings and grand rounds, were suspended.11 Formal teaching, such as regional training days, simulation training and mandatory courses such as Advanced Life Support (ALS), were also temporarily suspended in some, but not all, UK regions. This variability across different regions of the UK may have caused trainees to be concerned about the influence of geographical location on their training. There were dramatic disruptions to the traditional model of teaching, moving away from didactic learning such as lectures and tutorials to adopting emerging technologies for virtual online learning.12 A rapid implementation of communication software technology such as Microsoft Teams and Zoom were rapidly adopted to facilitate interactive webinars and video-conferencing. Utilisation of these technology platforms enhanced accessibility of online teaching and video conferencing from home or workplace leading to increased opportunity for trainees to attend regional or national meetings that would otherwise have been logistically difficult.
The trainers have also been significantly affected by the pandemic. Teaching commitments were disrupted due to increased demand from clinical duties, and the teaching activities that continued were delivered via virtual platforms. This was a novel experience for all involved and not without its technological challenges.
Research
All healthcare workers made a collective effort to join the clinical workforce in tackling the COVID-19 pandemic. This has resulted in deferral, or even cancellation, of out of programme (OOP) duties for some trainees. Such duties included research and medical education as well as leadership and management roles. Much of the non-COVID related research during the first peak of COVID-19 was suspended, with closure of laboratories and a halt in patient recruitment and visits.2 Research that was due to be presented at both national and international conferences was largely deferred or cancelled. Unfortunately, this has made it difficult for certain trainees to share their work, learn about other exciting work in the same field, and hindered some collaborative and networking opportunities. On the other hand, the COVID-19 pandemic has inspired many trainees who are often unfamiliar with research to be involved in ground-breaking work such as the Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial, which has contributed to the current standard of care for COVID-19 patients in the UK.13
Leadership
Many junior doctors have limited formal teaching in leadership during their medical training.14 This is despite leadership having been identified by the GMC as an essential skill that should be taught in all postgraduate medical training.15 The King’s Fund 2010 report on the leadership needs of clinical directors stated that leadership was an important skill doctors needed to master as future healthcare leaders.16
The COVID-19 pandemic has created the opportunity for healthcare workers to lead at local and national spheres in order to meet healthcare demands.17 Leadership in uncertain times (in the context of cancelled examinations, deferred rotations and redeployment to unfamiliar clinical specialties) requires quick thinking and adaptability to novel conditions, an attribute known as ‘adaptive leadership’.18 Flexibility of trainees to undertake roles previously performed by other team members has allowed them to gain better appreciation for teamwork. Innovation and rapid reconfiguration of healthcare services has led to accelerated uptake of telemedicine.19 For doctors, many face-to-face clinics have been replaced by novel platforms of tele-consulting, which were unfamiliar to many and have forced them to quickly adapt to an unorthodox service delivery. Furthermore, leadership in delivering clinical care has faced challenges. Many doctors had to engage in difficult conversations about escalation of care for patients with COVID-19 infection, a situation compounded by lack of knowledge of this new disease and its clinical progression and prognosis.18
Health Education England recently published ‘The Future Doctor Programme Report’ which sets out how medical education is likely to reform so that future doctors are equipped with the right attributes and skills to respond to an ever-changing healthcare landscape.20 Leadership, followership and team building were identified as imperative skill sets for future doctors. This report is particularly pertinent in the context of the current COVID-19 pandemic.
Progression
As part of the contingency plan to mitigate the risks of having face-to-face interviews, the Physician Specialty Recruitment Office (PSRO) have had to revise the recruitment process, as outlined in Table 1. Before COVID-19, candidates’ self-assessed short-listing scores accounted only for 20% of the final score and the evidence provided by candidates verified at the interview contributed to the remaining 80% of the final score. After interviews were cancelled, the revised PSRO model relied completely on the self-assessed short-listing scores without verifying evidence of accomplishments in what was called a ‘high-trust model’. Furthermore, the new assessment model removed five of the short-listing score domains from the initial ranking and adjusted the weighting of the other five based on, yet to be published, analysis that postulated that only the selected five domains correlated to trainees’ performance in the interview and appointability rates.
Table 1 Physician Specialty Recruitment Office (PSRO)-coordinated specialty recruitment – COVID-19 contingency arrangements. Adapted from Physician ST3 Recruitment, 2020.36
|
|
|
|
|
|
|
Quality improvement
|
Yes
|
10
|
1.2
|
1
|
|
Teaching experience
|
Yes
|
7
|
1.0
|
2
|
|
MRCP(UK)
|
ST3 only
|
12
|
1.0
|
3
|
|
Training in teaching
|
Yes
|
5
|
1.0
|
4
|
|
Presentations
|
Yes
|
8
|
1.5
|
5
|
|
Publications
|
No
|
8
|
N/A
|
6
|
|
Additional undergraduate degrees
|
No
|
6
|
N/A
|
7
|
|
Prizes/awards
|
No
|
8
|
N/A
|
8
|
|
Leadership and management
|
No
|
8
|
N/A
|
9
|
|
Postgraduate qualifications
|
No
|
8
|
N/A
|
10
|
The British Junior Cardiologists’ Association (BJCA) starter committee analysed the self-assessment scores of 117 trainees. They argued that the PSRO model failed to mimic the conventional interview process by only relying on variations in ‘Training in Teaching’ and ‘Quality Improvement Projects (QIPs)’, which are mandatory projects for trainees to identify issues in an area of clinical practice and implement changes that improve patient care, to discriminate between candidates. The revised model produced a negatively skewed cohort of candidates with very close overall scores, meaning that the slightest change in scores could lead to marked alterations in the ranking.21 This has significantly disadvantaged trainees who have had substantial leadership or research backgrounds and those who have not yet had the opportunity for formal training in teaching. Moreover, ‘Commitment to Specialty’, which was previously a key determinate for scoring highly at interview, was disregarded.
These highlighted concerns led PSRO to change the process of the second recruitment round where virtual interviews and a stringent process to validate evidence of accomplishments were introduced. However, conducting virtual interviews carries further challenges and concerns. First, both interviewers and candidates may not be familiar with the chosen teleconferencing platform, which may hinder performance for the candidate and evaluation from the interviewer. Second, candidates may not be able to comprehensively demonstrate their interpersonal and soft skills. Thirdly, there is a risk of bias against candidates based on their socioeconomic status as video interviews may reveal insights into the candidate’s personal environment.22
There is no doubt that many high-achieving candidates have failed to secure their wished-for posts due to the impact of COVID-19 on higher specialty recruitment.23 This caused significant distress amongst these trainees, adding more pressure on a medical workforce already suffering from substantial shortages. In 2018, the RCP carried out a census of consultant physicians and higher specialty trainees that revealed that 43% of advertised consultant posts were under-filled due to a lack of suitable applicants and 40% of consultants commented that rota vacancies occurred on a daily or weekly basis.24 It is possible that these findings may have been further accentuated by the pandemic.
Safety and wellbeing
A recent study found that front-line healthcare workers have a threefold increased risk of acquiring COVID-19 infection compared with the general population. Adequate PPE reduced but did not eradicate this risk.25 The study reported that the risk of having a positive COVID-19 test was higher among healthcare workers in the UK compared with their American counterparts.25 Two UK surveys investigated the possible causes behind this observation. The first was a survey across 18 UK Foundation Schools that showed that 74% of doctors received no formal training on managing COVID-19.26 The second was a British Medical Association (BMA) survey in which half of all doctors, working in high-risk areas, reported shortages or no supply of PPE and 50% said that they felt pressurised to work in a high-risk area. Respondents to the survey describe sourcing their own PPE from local schools, do it yourself (DIY) stores or voluntary groups.27 The lack of PPE at the start of the pandemic was a critical issue, and contributed significantly to trainee wellbeing and safety; many doctors felt they were putting themselves in harm’s way with suboptimal protection.
The presence of burnout amongst physicians and trainees has been well documented in previous pandemics.28,29 Increased workload, high levels of uncertainty, lack of control, and social isolation contributed to trainees and trainers having considerable psychological distress.30 The trainees and their trainers who worked on the front line have experienced extreme anxiety with intense emergency rotas and fears of possible infection; all of which have put them at risk of emotional, mental and physical exhaustion. Trainee and trainer burnout not only jeopardises their wellbeing, but is also associated with increased medical errors and substandard quality of patient care.
Clinically vulnerable trainees who required shielding have also been affected by the COVID-19 pandemic. Feeling guilty over leaving colleagues on the front line of clinical care may have aggravated the stress and anxiety of isolation as well as the uncertainty around training.31,32 When shielding was no longer advised, trainees expressed their concerns about returning to work as some of them felt unsupported or even ‘forgotten’.33 Trusts and supervisors should therefore ensure a safe and smooth transition back to work for shielded trainees while focusing on their wellbeing and unmet training needs. Training educational supervisors to support returning trainees will increase the consultant trainer’s confidence in addressing the challenges faced by the trainees.34
Although the focus of this review has been the impact of the COVID-19 pandemic on internal medicine training in the UK from a trainee perspective, it is important to appreciate the considerable impact on trainers too. The GMC’s National Training Survey of October 2020 highlighted that almost four-fifths of trainers saw their work change significantly in the peak of the first wave35 and 78% of trainers felt that their role as a trainer was disrupted due to the COVID-19 pandemic.35 It is important not to underestimate the pressures that trainers have experienced during this pandemic and its impact on internal medicine training; indeed, a ‘burnt out’ trainer is likely to be less effective at training.
Getting ready for the next wave: future considerations
Based on the experience of living with COVID-19, it seems likely that there will be a continued and prolonged course of tightening followed by relaxing of restrictions. It remains uncertain how long the changes to the internal medicine training programme will continue to be implemented. Adaptation to this new situation is necessary to prepare future clinicians for medical practice.
The COVID-19 pandemic has forced rapid adjustments to medical education and clinical training. Since changes introduced during this pandemic may continue longer than expected, there is a need to evaluate their effectiveness and the repercussions on trainees in the future. Reshaping and easing of certain ARCP standards raise the issue of quality assurance with the imperative requirement to ensure the standard of competence for trainees is not compromised. On a positive note, new avenues of learning opportunities have emerged as a consequence of this pandemic; namely the use of virtual learning platforms in disseminating knowledge and learning beyond the previously determined internal medicine confines as well as continuing to engage in novel research and leadership opportunities. Table 2 outlines the main challenges discussed in this paper and proposed solutions.
Table 2 COVID-19 – impact/challenges and potential solutions/adaptations
| |
|
|
|
Training
|
- Missed placements that were mandatory (geriatrics/ICU) or a specialty of interest
- Cancelled MRCP exams in second sitting of 2020
- Tele-clinics limit possibilities of face-to-face observation and WPBAs
- Reduction in elective non-urgent procedures such as endoscopy/lumbar punctures/chest drains resulting in de-skilling and fewer learning opportunities for trainees
|
- Flexibility in placement allocation in IMT Year 3
- Re-commencement of MRCP Part 1 and 2 through online MCQ format and PACES with a new format, including virtual consultations and PPE
- IMT curriculum to include specific training in tele-clinics/virtual consultations and clinic-based WPBAs
- Implement more virtual simulation training in IMT curriculum
|
|
Teaching
|
- Regional teaching, departmental meetings and national conferences cancelled
- Key national courses such as Advanced Life Support (ALS) course cancelled
|
- Video-conferencing portals to facilitate and deliver formal teaching, meetings and conferences
- Re-commence mandatory courses that are required for trainee progression
|
|
Research
|
- Halt in non-COVID related research
- Academic trainees deployed to the front line and faced considerable challenges to their research
|
- All academic trainees should have an assessment of the disruption to their research and clinical training needs
- To provide realistic time schedules for re-starting research and flexibility for periods of extension
|
|
Progression
|
- ARCP competencies not met
- Specialty recruitment process altered. Many recruited purely on their self-assessed short-list score and having no interview
|
- ARCP competencies need to be reviewed and made more flexible
- Amendment of PSRO-coordinated specialty recruitment based on feedback. Virtual interviews for specialty recruitment
|
|
Leadership
|
- Disruption(s) in OOP leadership and management roles
|
- Stronger emphasis on leadership and followership in IMT curriculum and mandatory teaching
|
|
Safety and wellbeing
|
- Lack of PPE putting trainees at increased risk of COVID-19 infection
- Trainee anxiety and burnout
- Shielding groups returning to work after prolonged absence from clinical placement
- Workplaces not supporting social distancing
|
- If PPE is rationed, importance on protecting trainees working in high-risk areas
- Ensure counselling and support services are easily accessible and of high quality
- Supportive return to work period and workplace risk assessments to ensure safe working conditions
- Encourage peer support and online networking for non-judgmental listening
|
Conclusion
‘In a time of drastic change, it is the learners who inherit the future. The learned usually find themselves equipped to live in a world that no longer exists.’
This quote by Eric Hoffer has never been more relevant. The changes in training posed by the pandemic are likely to persist in the foreseeable future and ensuring that internal medicine training keeps up with these changes is imperative. After all, today’s trainees are tomorrow’s trainers. 
Acknowledgements
The authors would like to acknowledge the hard-work, dedication and sacrifice of all healthcare workers during these unprecedented times.
References
1 General Medical Council (GMC). Joint statement: Supporting doctors in the event of a COVID-19 epidemic in the UK. 2020. https://www.gmc-uk.org/news/news-archive/supporting-doctors-in-the-event... (accessed 03/03/21).
2 Alvin MD, George E, Deng F et al. The impact of COVID-19 on radiology trainees. Radiology 2020; 296: 246–8.
3 Yuen J, Xie F. Medical education during the COVID-19 pandemic: perspectives from UK trainees. Postgrad Med J 2020; 96: 432–3.
4 Hettle D, Sutherland K, Miles E et al. Cross-skilling training to support medical redeployment in the COVID-19 pandemic. Future Healthc J 2020; 7: e41–4.
5 General Medical Council (GMC). GMC asked to register further groups of doctors. 2020. https://www.gmc-uk.org/news/news-archive/gmc-asked-to-register-further-g... (accessed 03/03/21).
6 Health Education England. Two thousand new doctors sign up to join COVID-19 battle ahead of schedule. 2020. https://www.hee.nhs.uk/news-blogs-events/news/two-thousand-new-doctors-s... (accessed 03/03/21).
7 Hinchliffe G. Should we really be using final year medical students to bolster the coronavirus front line? BMJ. 2020. https://blogs.bmj.com/bmj/2020/04/30/should-we-really-be-using-final-yea... (accessed 03/03/21).
8 Joint Royal College of Physicians Training Board. Curriculum for Internal Medicine Stage 1 Training. JRCPTB. 2019. https://www.jrcptb.org.uk/sites/default/files/Internal%20Medicine%20stag... (accessed 03/03/21).
9 Joint Royal Colleges of Physicians Training Board. JRCPTB 2020. Requirements for outpatient experience in internal medicine training. https://www.jrcptb.org.uk/news/outpatient-clinic-experience-and-training... (accessed 15/06/20).
10 Physician ST3 recruitment. Am I eligible. 2019. https://www.st3recruitment.org.uk/recruitment-process/am-i-eligible/mrcp-uk (accessed 03/03/21).
11 Arandjelovic A, Arandjelovic K, Dwyer K et al. COVID-19: Considerations for Medical Education during a Pandemic. MedEdPublish 2020: 10.15694/mep.2020.000087.1.
12 Goh P-S, Sandars J. A vision of the use of technology in medical education after the COVID-19 pandemic. MedEdPublish 2020: 10.15694/mep.2020.000049.1.
13 Van’t Hoff. Building back better research post covid-19. BMJ. https://blogs.bmj.com/bmj/2020/08/26/building-back-better-research-post-... (accessed 03/03/21).
14 Perry J, Mobley F, Brubaker M. Most doctors have little or no management training, and that’s a problem. Harvard Business Review, 2017. https://hbr.org/2017/12/most-doctors-have-little-or-no-management-traini... (accessed 03/03/21).
15 General Medical Council (GMC). Generic professional capabilities framework, 2017. https://www.gmc-uk.org/-/media/documents/generic-professional-capabiliti... (accessed 03/03/21).
16 Giordano R. Leadership of needs of medical directors and clinical directors. London: King’s Fund, 2010. https://www.kingsfund.org.uk/sites/default/files/Leadership-needs-clinic... (accessed 03/03/21).
17 Gupta AK, Neely J,Wilkinson C. Clinical leadership training: a clinician’s perspective. Clin Radiol 2020; 76; 241–6.
18 Warraich S, Olabi B, Azhar B et al. Medical leadership in the NHS during the COVID-19 pandemic. Br J Hosp Med 2020: 81; 1–3.
19 Peek N, Sujan M, Scott P. Digital health and care in pandemic times: impact of COVID-19. BMJ HCI 2020; 27: 1–3.
20 Health Education England. Future Doctor. https://www.hee.nhs.uk/our-work/future-doctor (accessed 03/03/21).
21 Bradley-Watson J, Samways JW, Allen CJ et al. Understanding trainee physician specialty recruitment during covid-19: insights from a trainee lead survey. http://www.bcs.com/documents/BJCA_ST3_Report_Final_Clean_BJCA_09_06.pdf (accessed 03/03/21).
22 Davis MG, Haas MRC, Gottlieb M et al. Zooming in versus flying out: virtual residency interviews in the era of COVID-19. AEM Education and Training 2020; 4: 443–6.
23 Rimmer A. Physician trainees raise concerns about modified recruitment process. BMJ 2020; 369: m2038.
24 RCP London. Focus on physicians: 2018–19 census (UK consultants and higher specialty trainees). https://www.rcplondon.ac.uk/projects/outputs/focus-physicians-2018-19-ce... (accessed 03/03/21).
25 Nguyen LH, Drew DA, Graham MS et al. Risk of COVID-19 among front-line healthcare workers and the general community: a prospective cohort study. Lancet Public Health 2020; 5: e475–83.
26 Blackburn B, Ferryman JT, Alattas A. Impact of COVID-19 on UK Foundation Doctors: training and safety. Research Square 2020: 10.21203/rs.3.rs-30834/v1.
27 BMA Media Team. BMA survey reveals almost half of doctors have relied upon donated or self-bought PPE and two thirds still don’t feel fully protected. BMA, 2020. https://www.bma.org.uk/bma-media-centre/bma-survey-reveals-almost-half-o... (accessed 03/03/21).
28 Kisely S, Warren N, McMahon L et al. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ 2020; 369: m1642.
29 Spoorthy MS. Mental health problems faced by healthcare workers due to the COVID-19 pandemic – a review. Asian J Psychiatr 2020; 51: 102119.
30 Wu PE, Styra R, Gold WL. Mitigating the psychological effects of COVID-19 on health care workers. CMAJ 2020; 192: E459–60.
31 Iliff HA, Simpson KA, Tomlinson CR et al. ‘Shielded’ anaesthetists and intensivists during the COVID-19 pandemic. Anaesthesia 2020; 75: 1541–2.
32 Rimmer A. How can I help shielded trainees return to work? BMJ 2020; 370: m3188.
33 Rimmer A. Covid-19: shielding doctors express concerns about returning to work. BMJ 2020: 370; m2918.
34 Hallewell R, Bryant C, Deaner A et al. Training educational supervisors to support physician trainees returning to practice. Future Healthc J 2020; 7: 120–4.
35 General Medical Council. National training survey, 2020. https://www.gmc-uk.org/-/media/documents/nts-results-2020---summary-repo... (accessed 03/03/21).
36 PSRO-coordinated specialty recruitment - COVID-19 contingency arrangements [press release]. 2020. https://www.st3recruitment.org.uk/documents (accessed 15/08/20).