In Stone Age times, our hunter gatherer ancestors needed to be physically fit in order to survive. They well knew the need to develop sufficient strength, power and dexterity to avoid threats, seize opportunities for survival and find food and shelter. Fast forward several hundred thousand years, and how socialisation has changed. In 2020, the World Health Organization advocated at least 150-300 minutes of moderate to intense exercise per week for adults,1 typically walking, running, or swimming.
Physical activity is voluntary body movement resulting in energy expenditure. Exercise is a planned physical activity involving purposeful movement, with one of its main advantages being maintenance or improvement of physical and mental health. While we should aim to adopt regular exercise into our daily lives, benefit is observed even when little or no physical activity is replaced by any increase.2 Across the world, one in four adults fail to meet recommended levels of exercise,3 while more than 80% of adolescents are insufficiently physically active.4 Prior to the COVID-19 pandemic, data from England found that around 25% of the adult population were inactive (defined as exercising for less than 30 minutes each week).5 Demographics associated with being inactive included increasing age, lower socioeconomic status, and having a disability or long-term health condition.5
The UK national lockdown was announced in late March 2020. Advice was to “stay at home” and exercise outside once a day, alone or with household members (with similar, but in some locations more stringent, advice given in many other countries). Such legislation is therefore likely to have reduced the amount of time spent being active. Moreover, increased working from home, closure of gyms, tennis courts, sports halls and swimming pools, little or no organised individual or group sport activities and home schooling will have compounded the time being sedentary. This is all of additional concern as it is known that obesity increases the chance of being admitted to hospital with COVID-19, with the highest death rates occurring in countries with the highest prevalence (of obesity).6
In the months following declaration of a global pandemic, people across the world decreased their activities and travelled less. In the UK, device-tracked activity levels declined by a median of 37%, with 63% of people overall decreasing their activity, although adults aged >70 years were more likely to maintain physical activity levels.7 Alarming findings were observed in children, as one Dutch study of objectively measured activity levels demonstrated that in the summer before the pandemic, 64% of children achieved recommended physical activity levels versus only 20% in 2020.8
Regular exercise confers almost immediate, medium, and long-term benefits. Not exercising, on the other hand, is hazardous to health. In one meta-analysis of 34 cohort studies (involving well over a million individuals), being sedentary had a dose-dependent association with all-cause mortality, increasing disproportionately with less activity.9 Similarly, a meta-analysis of 14 cohort studies (involving 232,149 individuals) reported a 27% reduction in all-cause mortality associated with running; this included 30% related to cardiovascular disease and 23% to cancer.10 Moreover, in a further large study incorporating 16 meta-analyses (305 randomised controlled trials overall), regular exercise reduced mortality in coronary heart disease, stroke, and pre-diabetes more than any of the drugs used in these conditions (except diuretics in heart failure).11 The positive impact of pulmonary rehabilitation in chronic obstructive pulmonary disease is well embedded in guidelines where participation results in fewer symptoms and greater walking distance. With regular exercise, data have also demonstrated a lower incidence of depression12 and cognitive benefits in adolescents and young adults.13In the older population, exercise can decrease the risk of falling.14Exercise-based interventions can be helpful in reducing fatigue and increasing quality of life in advanced cancer,15 while the incidence of cancers such as breast, colorectal, lung, gastric, endometrial, and bladder cancer is lower in those who exercise regularly.16
Even outwith periods of enforced regional and national lockdowns, countless barriers exist to engagement in regular exercise. Many of these are complex and involve an interplay between individuals, resource, and society, while such intricately woven barriers vary according to age, socioeconomic status, ethnicity and past experiences.17 Nevertheless, many motivators such as weight loss, enhanced mood, social engagement, maintaining physical fitness and management of a pre-existing medical disorder do exist. Is it possible that incentives such as these are overlooked, poorly understood or not perceived to be sufficiently rewarding?
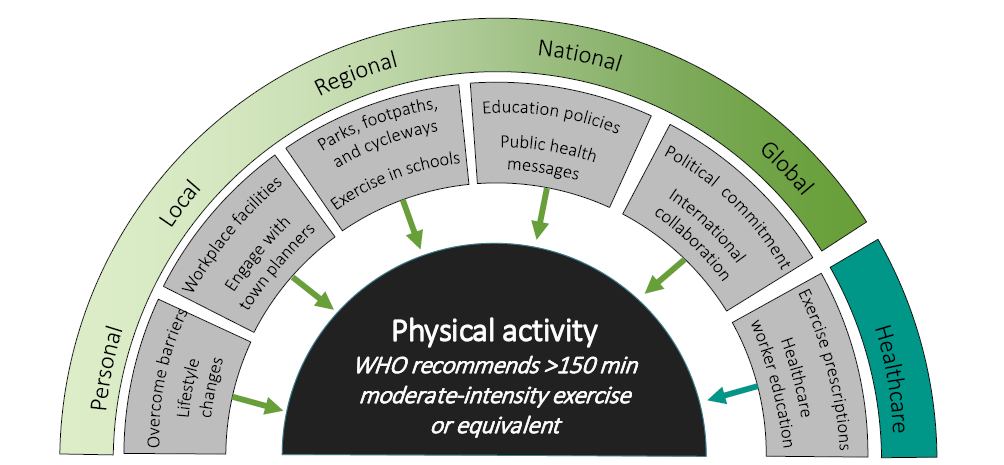
Mass education, sustained public health messages, change in political policy and re-shaping of society and its infrastructure must all surely form keystones towards encouraging populations to be more physically active (Figure 1). Making physical activity fun and accessible is also likely to enhance engagement. A popular example of this is the regularly streamed exercise package provided by the UK’s ‘favourite physical education instructor’ Joe Wicks, with a following of over two million on YouTube. Similarly, the NHS ‘couch-to-5k’ programme is available for free and accessible to all.18 A less digital example is the widespread introduction of ‘park runs’, endorsed by the Royal College of General Practitioners, which involve free weekly five-kilometre events across the four nations of the UK, supported by local volunteers. Moreover, it is imperative that each and every healthcare professional and healthcare delivering body helps address the impending sedentary crisis by vociferously ‘shouting out loud’ that illness prevention is better than cure, and that being physically active is pivotal to such a process. Healthcare professionals can also prescribe physical activity19 although more widespread education on how to do this is essential, as well as a greater emphasis in undergraduate curricula on the integral role of physical activity in health.
Figure 1 Strategies by which to encourage engagement in exercise
We need to embrace technology and develop interactive, individualised, automated, and evidence-based tools to support exercise in the longer term. We all need to understand that regular exercise is the panacea of many ills. And we all need to appreciate that it maintains and improves the physical and mental well-being of the well, and through its use we can improve not only the physical and mental well-being of our patients, but of ourselves too. From the leaders of all nations and political parties implementing policy change, to sustained ‘loud and clear’ public health messages, to the elderly ‘getting on their (e-) bikes’ and down to nursery school children walking to school, we all have a role to play in helping turn the tide of another of the unintended by-products of enforced lockdown. All eyes are turned towards health and economic recoveries following the COVID-19 pandemic, but we must not lose sight of the perils of being sedentary and the many benefits that come from regular exercise. Now is the time to engage. Let us not forget what lessons Stone Age man and woman can teach us with regards to the importance of moving. 

References
1 World Health Organization. WHO guidelines on physical activity and sedentary behaviour. Geneva: World Health Organization; 2020.
2 Hupin D, Roche F, Gremeaux V et al. Even a low-dose of moderate-to-vigorous physical activity reduces mortality by 22% in adults aged ≥60 years: a systematic review and meta-analysis. Br J Sports Med 2015; 49: 1262-67.
3 Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Health 2018; 6: e1077-e86.
4 Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child & Adolesc Health 2020; 4: 23-35.
5 Sport England. Active Lives Adult Survey. November 17/18 Report. London: Sport England; 2019.
6 World Obesity. COVID-19 and Obesity: The 2021 Atlas. London: World Obesity Federation; 2021.
7 Tison GH, Avram R, Kuhar P, Abreau S, Marcus GM. Worldwide effect of COVID-19 on physical activity: a descriptive study. Ann Intern Med 2020; 173: 767-70.
8 ten Velde G, Lubrecht J, Arayess L, et al. Physical activity behaviour and screen time in Dutch children during the COVID-19 pandemic: Pre-, during- and post-school closures. Pediatr Obes 2021; e12779.
9 Patterson R, McNamara E, Tainio M, Herick de Sa T, Smith AD, Sharp SJ et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol 2018; 33: 811-29.
10 Pedisic Z, Shrestha N, Kovalchik S, Stamatakis E, Liangruenrom N, Grgic J et al. Is running associated with a lower risk of all-cause, cardiovascular and cancer mortality, and is the more the better? A systematic review and meta-analysis. Br J Sports Med 2020; 54: 898-905.
11 Naci H, Ioannidis JPA. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ 2013; 347: f5577.
12 Gianfredi V, Blandi L, Cacitti S, Minelli M, Signorelli C, Amerio A et al. Depression and objectively measured physical activity: a systematic review and meta-analysis. Int J Environ Res Public Health 2020; 17: 3738.
13 Haverkamp BF, Wiersma R, Vertessen K, van Ewijk H, Oosterlaan J, Hartman E. Effects of physical activity interventions on cognitive outcomes and academic performance in adolescents and young adults: A meta-analysis. J Sports Sci 2020; 38: 2637-60.
14 Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev 2019; 1: CD012424.
15 Dittus KL, Gramling RE, Ades PA. Exercise interventions for individuals with advanced cancer: A systematic review. Prev Med 2017; 104: 124-32.
16 Ziebart C, McArthur C, Lee L, Papaiannou A, Laprade J, Cheung AM et al. “Left to my own devices, I don’t know”: using theory and patient-reported barriers to move from physical activity recommendations to practice. Osteoporos Int 2018; 29: 1081-91.
17 Crooke R, Haseler C, Haseler T, Collins J, Crockett A. Physical activity and moving more for health. J R Coll Physicians Edinb 2020; 50: 173-80.
18 National Health Service. Get running with couch to 5K [Internet]. [Accessed 13 May 2021]. Available from: www.nhs.uk/live-well/exercise/get-running-with-couch-to-5k/
19 Moving Medicine [Internet]. [Accessed 13 May 2021]. Available from: www.movingmedicine.ac.uk